Equity and Quality at Independent Practices in LA County
December 5th, 2022
Launched in 2023, Equity and Quality at Independent Practices in LA County (EQuIP-LA) was a two-year improvement collaborative led by the California Quality Collaborative (CQC) dedicated to reducing disparities of care experienced by Medi-Cal enrollees of color.
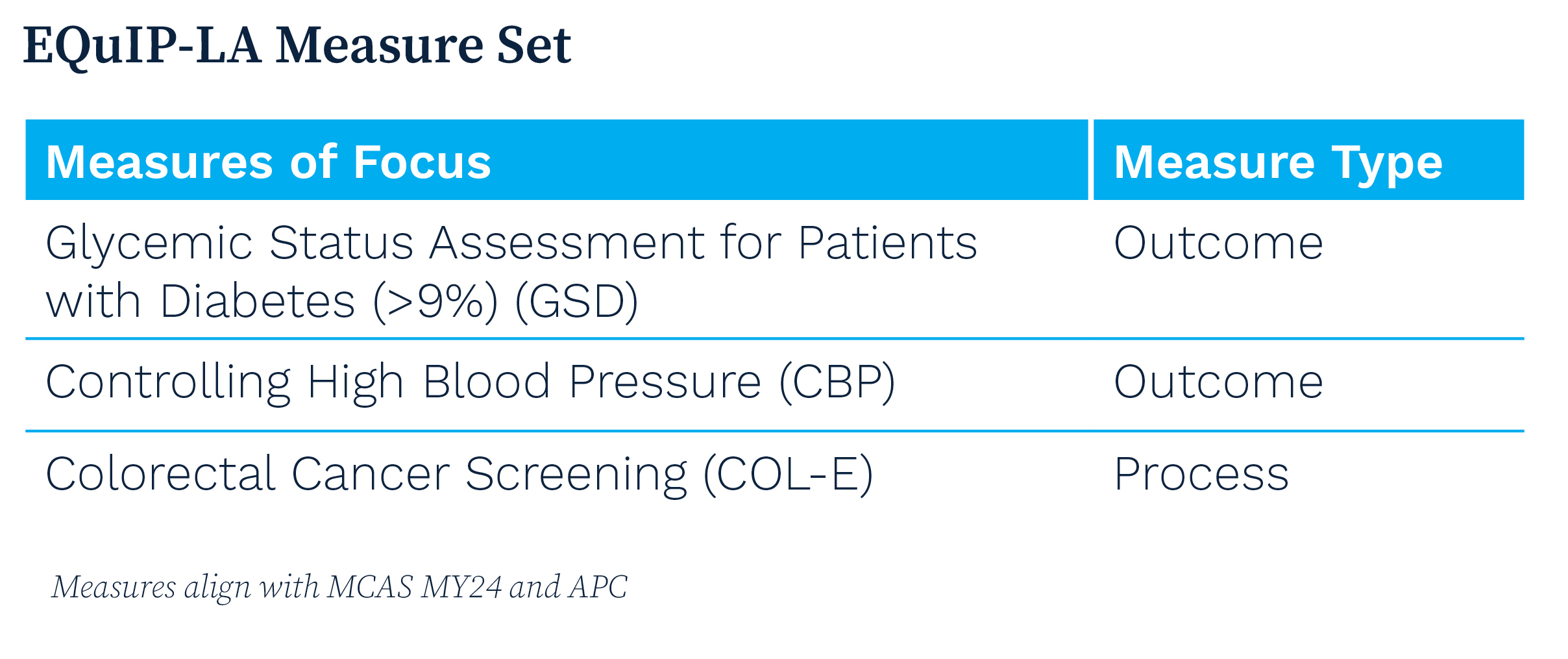
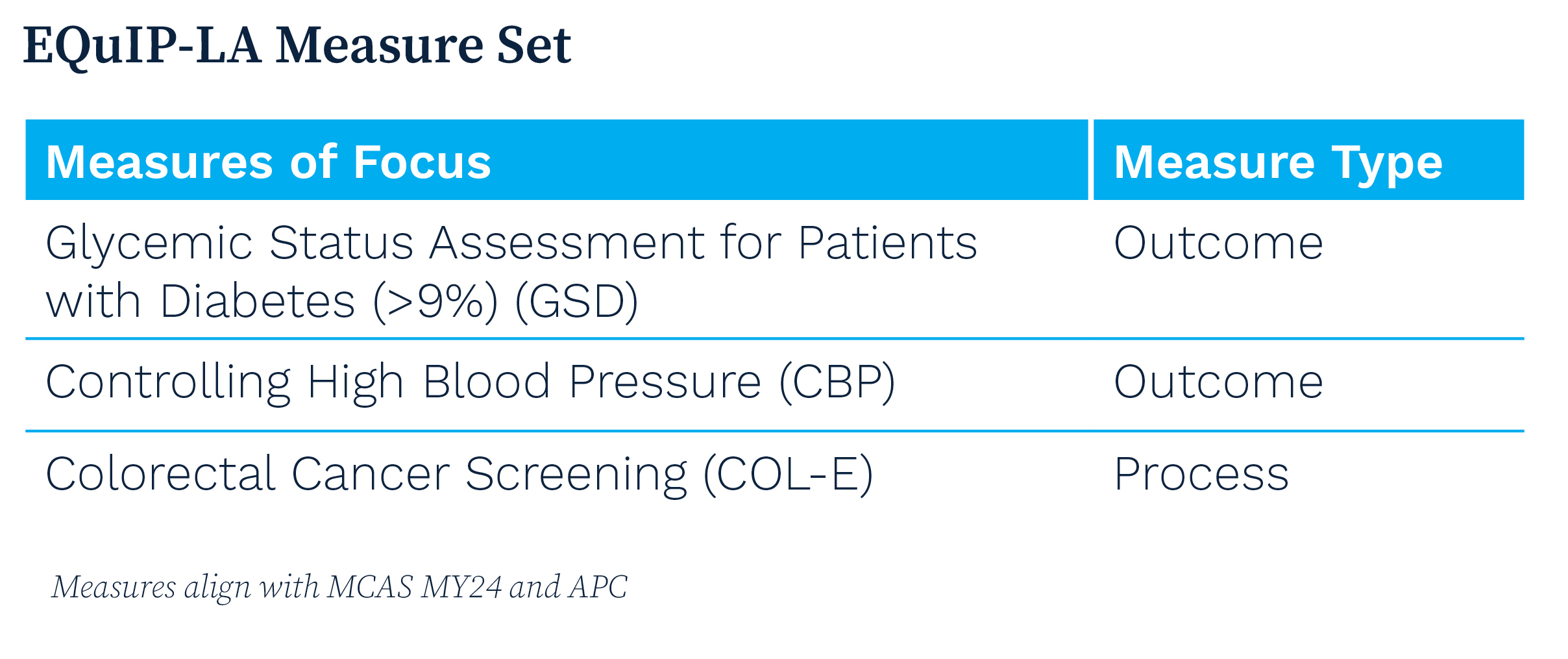
EQuIP-LA is supporting participating organizations by:
- Building their capacity and that of community-based practice coaches to implement an equity-centered approach to quality improvement
- Incorporating patients’ lived experiences into the co-design of the collaborative’s curriculum
- Designing and implementing interventions to address disparities of care related to chronic disease management and preventative screening, focusing on diabetes, hypertension and colorectal cancer screening
- Advancing the practice capabilities necessary for delivering advanced primary care
Participating Organizations
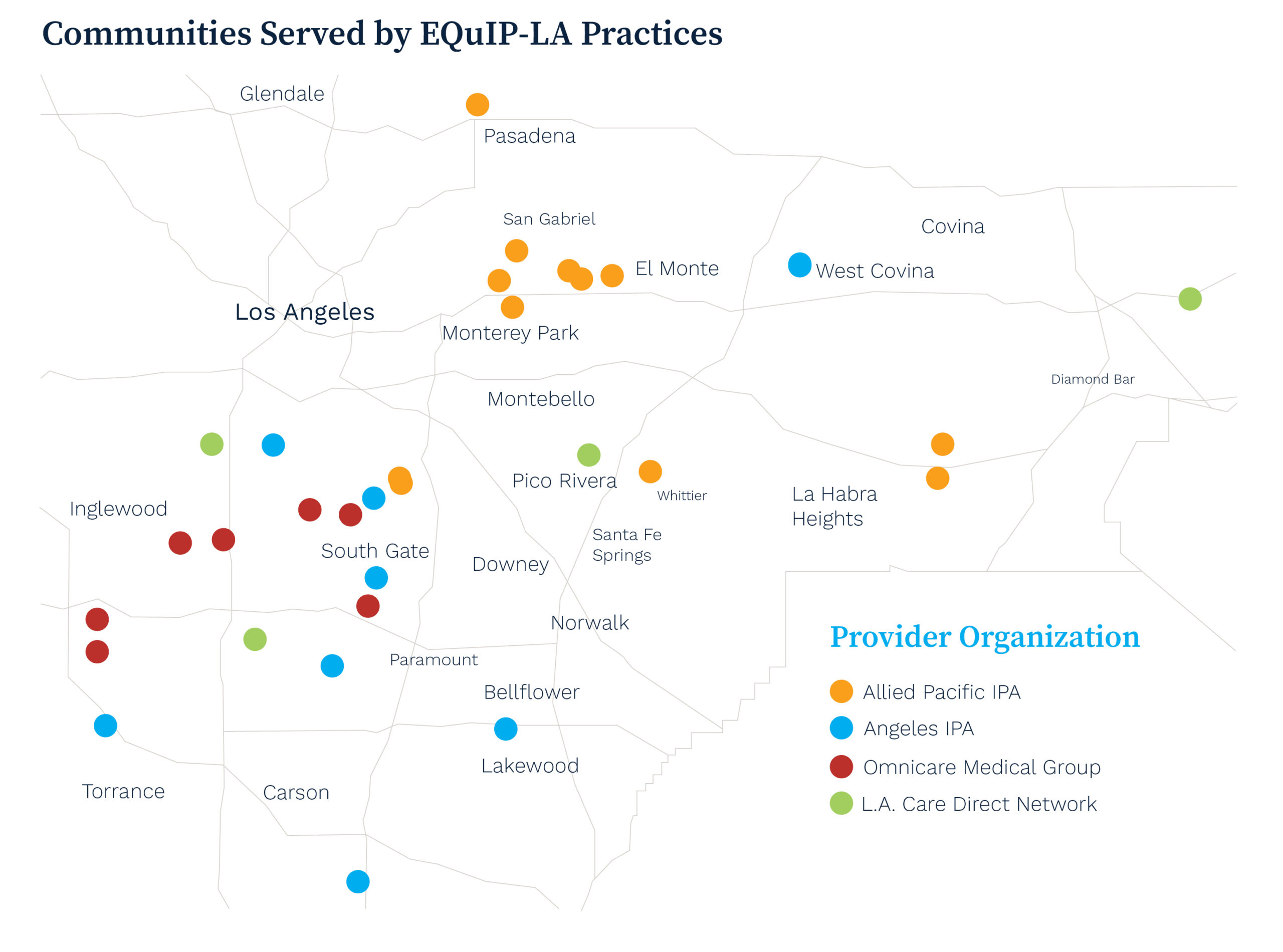
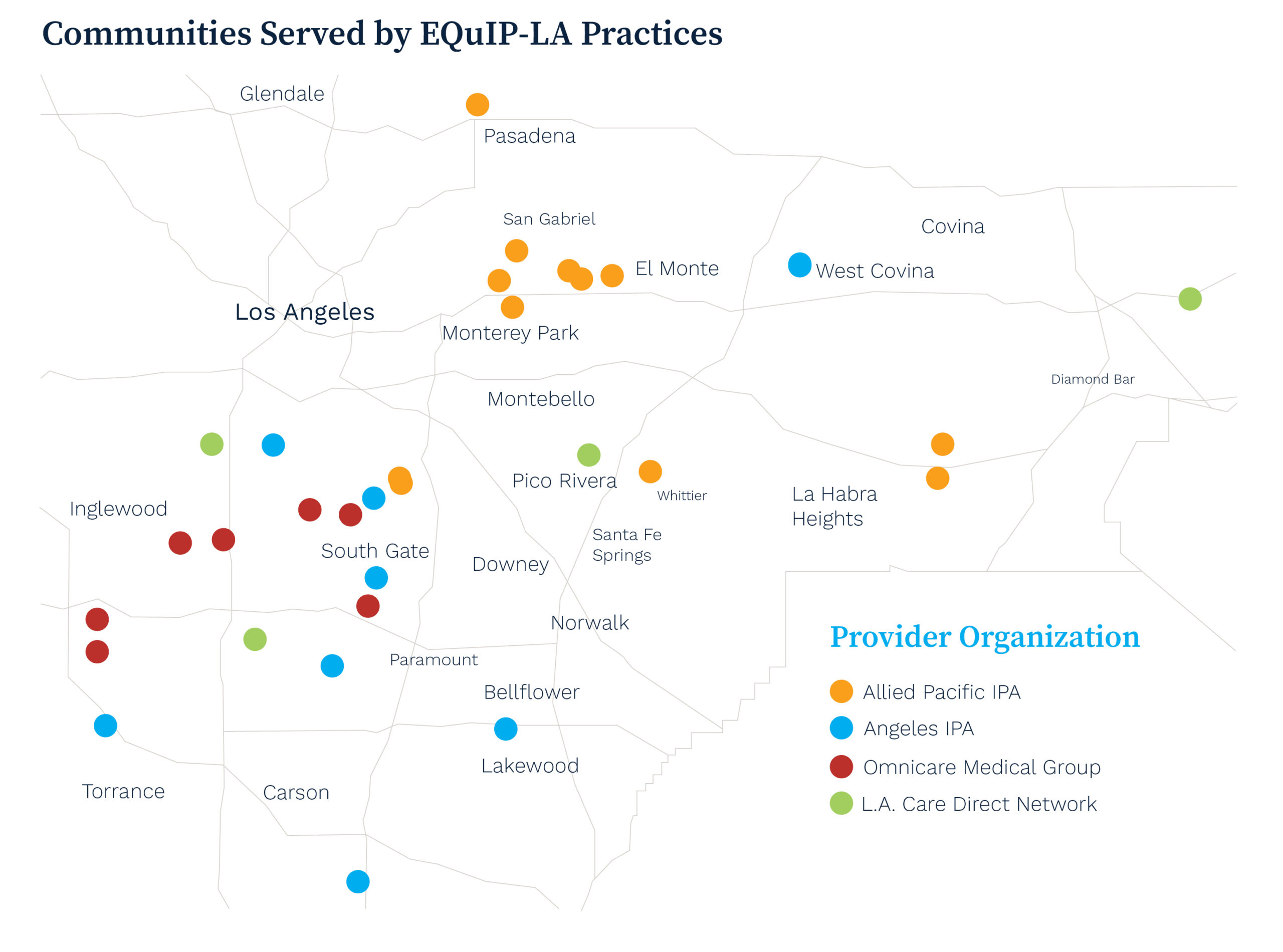
Four organizations committed to advancing health equity are participating in EQuIP-LA, serving more than 41,000 Medi-Cal enrollees, including over 30,000 individuals of color across Los Angeles County:
- Allied Pacific IPA — network of medical professionals serving the San Gabriel Valley
- Angeles IPA — multi-specialty network serving communities across Los Angeles and Orange Counties
- LA. Care Direct Network — directly-contracted network of physicians with L.A. Care Health Plan
- Omnicare Medical Group — multi-specialty network providing quality health care to the citizens of Lynwood, Compton and surrounding communities
Technical Assistance and Impact
EQuIP-LA deploys a community-based coaching model — a scalable approach to build practice coach capacity within health care delivery organizations to help them deliver health equity-focused quality improvement interventions.
Comprehensive technical assistance provided to participants, includes:
- Direct Funding. Supporting infrastructure investments and projects to reduce health disparities for participating IPAs and their enrolled practices.
- Targeted Training. Utilizing evidence-based frameworks to support high-quality primary care, including the Model for Improvement and the 10 Building Blocks of Primary Care.
- Personalized Advising. Offering one-on-one needs assessment and improvement advising to define and implement IPA- and practice-specific quality improvement plans.
- Data Insights. Providing tools to support visualization and interpretation of performance data to identify improvement opportunities.
- Collaborative Learning. Facilitating regular opportunities to engage with peers from other organizations to share learnings and ideas.
Practice Stories of Transformation
The EQuIP-LA program collaborated with primary care practices across Los Angeles County to address disparities in chronic disease management and preventative care.
Tweedy Medical Group credits EQuIP-LA with invigorating their efforts to better serve their patients and greatly expanding their goals.
Reddy Care Medical relied on EQuIP-LA to greatly enhance care coordination and patient follow-up.
Elevating Patients’ Lived Experiences
EQuIP-LA has prioritized patient involvement from its inception, utilizing insights from a virtual patient listening session to inform its strategies. The session, facilitated by CQC and PFCCpartners, allowed Medi-Cal enrollees to share their experiences, directly shaping the program’s focus on timely access and culturally competent care. This approach ensures that interventions are tailored to meet the true needs of the communities served.
The collaborative’s ongoing implementation is supported by a steering committee made up of program partners, participants and a patient representative.
Partners
EQuIP-LA’s technical assistance is led by CQC. Collaborative partners include the California Health Care Foundation, Community Partners, PFCCpartners, HealthBegins, Health Net and L.A. Care Health Plan.
Support
EQuIP-LA is made possible thanks to the generous support of the California Health Care Foundation.
Improvement & Learning Collaboratives
November 7th, 2022
CQC’s improvement and learning collaboratives are multi-year programs offering technical assistance. Program participants receive personalized coaching from experts and engage in educational opportunities including virtual peer sharing, site visits and data analytics. These programs aim to foster a sustainable health care system accessible to all.
CalHIVE Behavioral Health Integration
October 24th, 2022
(more…)
Advanced Primary Care Resources
September 9th, 2022
Employers know that primary care is essential to a healthy workforce and employees’ access to a high-value health care system. Studies show that robust systems of primary care can lower overall health care utilization, disease and death rates and increase the use of preventive services. Strong primary care also may reduce the negative effects of income inequality and is associated with more effective and equitable health services.
For this reason, the Purchaser Business Group on Health (PBGH) has worked for the better part of the last decade to revitalize primary care. Through successive initiatives and in collaboration with a diverse group of committed stakeholders, PBGH has spearheaded efforts to create a blueprint for optimized primary care. The objectives are to fully utilize primary care’s potential to improve health outcomes, integrate behavioral health and reduce costs to the health care system.
Common Measure Set: A set of clearly defined health plan requirements and accountability expectations focused on advanced primary care.
Memorandum of Understanding for Payers: An agreement whereby organizations commit to increase investment in and access to advanced primary care.
Common Purchasing Agreements for Health Plans and Direct Contracting: Purchaser-endorsed standards to help achieve high-value equitable care.
Health Value Index: Specific performance indicators that create actionable insight into a purchaser’s health plan spending.
Advanced Primary Care Request for Information (RFI): PBGH has issued a collective RFI on behalf of our members to identify provider practices that meet established standards of advanced primary care and that are willing to partner. PBGH members will use these results in network design and/or in direct contracting arrangements.
California Advanced Primary Care Initiative
July 25th, 2022
The California Advanced Primary Care Initiative, a joint effort by CQC and the Integrated Healthcare Association (IHA), is a continuation of that effort to strengthen the primary care delivery system throughout the state by building and scaling a primary care model that emphasizes comprehensive, team-based and person-focused care, the integration of behavioral and physical health services and high-quality outcomes.
Multi-Payer Alignment
CQC and the IHA convened a coalition of large commercial health care payers to work together to enable primary care practices to transform to a high-performing, value-based care model that reduces costs and improves quality and equity. The payers currently participating are Aetna, Aledade, Blue Shield of California and Health Net.
These payers have signed a memorandum of understanding (MOU) committing to this coordinated effort through 2025. The MOU has four areas of focus:
1. Transparency: Report primary care investment, adoption of value-based payment models that support the delivery of advanced primary care and performance on the Advanced Primary Care measure set jointly developed by CQC and IHA.
2. Payment: Adopt an agreed upon value-based payment model for primary care providers that offers flexibility, supports team-based care delivery and incentivizes the right care at the right time.
3. Investment: Collaboratively set increased primary care investment quantitative goals without increasing the total cost of care.
4. Practice Transformation: Provide technical assistance to primary care practices working to implement clinical and business models for success in value-based payment models, integration of behavioral health and reduction of disparities.
Additional payer organizations are encouraged to sign onto the MOU and join this effort. Contact Lindsay Petersen to learn more.
EmployersRx 2022 Policy Agenda
June 13th, 2022
Our goal: Support Policies to Reduce Costs for All Purchasers While Encouraging Meaningful Innovation
End patent gaming. Support efforts to end gaming of patent and market exclusivity laws by drug makers.
- Eliminate “evergreening” and other “patent thickets” to ensure that branded products will face competition from generic drugs and biosimilars in line with the intent of current laws.
- Prevent first-to-file generic drug applicants from blocking, beyond a 180-day exclusivity period, the entrance of subsequent generic drugs to the market.
- Reduce citizens petition abuse by giving the FDA additional guidance on denying petitions submitted for the purpose of delaying generic approval.
- Require branded biologic companies to publicly list drug patents they can reasonably defend.
Transform the drug supply chain to ensure transparency and fair prices. Advocate for policies to bring fundamental change to the opaque and distorted drug supply chain.
- Continue to support policies designed to bring transparency to the drug supply chain, including requirements the Consolidated Appropriations Act of 2020 and the Transparency in Coverage rule placed on PBMs and others in the supply chain.
- Support new requirements for end-to-end price transparency placed directly on Pharmacy Benefit Managers (PBMs) and like organizations.
- Advocate for a comprehensive federal investigation of the drug supply chain, to include the financial and ownership relationships between PBMs; health insurers, group purchasing organizations; in-person pharmacies; mail-order specialty pharmacies; and affiliated organizations, including those based overseas.
- Establish a clear regulatory framework for PBMs and other organizations in the drug supply chain. This should include consideration of extending ERISA fiduciary responsibility to PBMs and affiliated organizations so that such entities are required to act in the best interest of plan sponsors and beneficiaries.
Support common-sense price transparency requirements for drugs sold to commercial employers.
- Require drug manufacturers to publicly report and explain price increases that exceed certain thresholds.
- Require health care providers and pharmacies to include National Drug Codes (NDC) in claims for commercial health plans. NDC codes are currently required for claims to public payers (Medicare and Medicaid) and provide greater transparency on prices to purchasers.
Oppose policies limiting purchasers’ ability to manage drug costs.
Other stakeholders have proposed policies that would limit the ability of employers and purchasers to manage their drug costs. These policies would further drive-up health costs for purchasers and families, and have no basis in clinical efficacy. EmployersRx will strongly oppose these policies which strip employers and purchasers of their already limited ability to manage their drug costs.
Support policies to catalyze the development and use of lower-priced biosimilars.
Employers and purchasers support the use of lower-priced biosimilar products. However, we do not support policies that further entrench the misguided Medicare Part B drug payment policy, which pays physicians to administer drugs based on their price.
Develop policies to address the very high cost of new specialty drugs.
Many new specialty drugs on the market or in development hold significant promise in the treatment or even cure of debilitating diseases. However, these drugs come with large price tags, significantly affecting employer drug spending. Policymakers should investigate and develop policies to address the very high cost of these drugs. Policies should focus on ensuring reasonable payment for highly effective therapies, while avoiding simply shifting how high-cost drugs are paid for, such as “drug mortgages” or other similar mechanisms.
Support comparative effectiveness research.
Support establishment and/or federal certification of independent comparative effectiveness entity/entities. Academic and empirical evidence demonstrates that drug prices are not meaningfully tied to the effectiveness of drugs in treating, curing, or managing disease. Private payers need this vital information to price drugs effectively. Prescription drug comparative effectiveness entities could be publicly operated, quasi-governmental, or non-profit, but must remain independent of manufacturers, health plans, PBMs, and other financially interested parties.
Continue to support fairness for private health plans in Medicare negotiation and inflation caps.
Continue to support inclusion of protections for private health plans in legislation enabling Medicare to negotiate the price of high-cost drugs and establish inflation caps on sole source drugs.
Contact CQC
January 4th, 2022
Use the contact information below to get in touch with CQC.
General Inquiries
Phone: (415) 281-8660
Email: CQCInfo@pbgh.org
Media Inquiries
Anna Elgart
aelgart@pbgh.org
415-615-6322
Emsana Health
October 24th, 2021

Emsana Health is PBGH’s Health Solutions Organization established by PBGH’s employer members who collectively spend $350 billion annually to provide health care benefits to 21 million Americans. Our work leverages PBGH’s deep expertise and it’s more than 30-year track record of incubating new, disruptive operational programs in partnership with large employers and other health care purchasers to lower health care costs and increase quality.
Emsana Health furthers PBGH’s charitable mission by commercializing and scaling solutions that increase employee access to high-quality health care and by lowering the health care spending that represents real opportunity costs for businesses and job growth for working Americans.
Products designed for employers
Emsana products have the backing of large employers and are designed to deliver sustained market change that benefits employers and the millions of Americans for whom they provide health benefits.
Our first product is EmsanaCare, a VIP Access Pass to the highest-quality health care. EmsanaCare makes it easy for private health care purchasers to identify and partner with advanced primary care practices and top-performing specialists to improve experience and health outcomes. EmsanaCare addresses the concerns of many large employers that the care they buy is difficult for employees to access, of uncertain quality and poorly integrated.
Learn more
EmployersRx 2021 Policy Agenda
April 20th, 2021
Support Policies to Reduce Costs for All Purchasers While Preserving Meaningful Innovation
Policymakers are considering a set of policies that use the Federal Government’s purchasing power to meaningfully reduce drug prices for beneficiaries and taxpayers. To ensure that these policies do not result in cost shifting to private payers, and to provide direct relief to families covered by private insurance, it is essential that any policies to directly manage drug prices extend to all payers, not just public programs. To that end, we urge policymakers to:
- Allow the federal government to enter into meaningful negotiations on the certain costs of drugs that lack sufficient competition. Negotiated prices must be available to all drug purchasers, not just Medicare. Negotiated prices should align with clinical efficacy, consider the price of the drug in other industrialized countries,and protect true innovation.
- Cap price inflation on existing drugs. The inflation cap must apply to all payers.
- Modify Medicare Part B to eliminate the incentive for providers to prescribe higher cost drugs.
Support Policies to Strengthen Competition and Enhance Transparency
Policymakers can take steps to indirectly reduce the cost of drugs by banning anticompetitive practices by drug makers and other actors, and enhancing price transparency. To that end, we urge policymakers to:
- Eliminate “patent evergreening” and other “patent thickets” to ensure that branded products will face competition from generic drugs and biosimilars in line with the intent of current laws.
- Prevent first-to-file generic drug applicants from blocking, beyond a 180-day exclusivity period, the entrance of subsequent generic drugs to the market.
- Reduce citizens petition abuse by giving the FDA additional guidance on denying petitions submitted for the purpose of delaying generic approval.
- Require drug manufacturers to publicly report and explain price increases that exceed certain thresholds.
- Require branded biologic companies to publicly list drug patents they can reasonably defend.
- Require health care providers and pharmacies to include National Drug Codes (NDC) in claims for commercial health plans. NDC codes are currently required for claims to public payers (Medicare and Medicaid) and provide greater transparency on prices to purchasers.
- Require complete transparency by pharmacy benefit managers and the pass through of all rebates and related fees and payments to plan sponsors.
- Address spread pricing by pharmacy benefit managers, health plans, providers, and other intermediaries. Purhasers should be given the option to accept or reject spread pricing. This policy should apply to drugs administered directly by providers and sold in the pharmacy setting.
Oppose Policies Limiting Purchasers’ Ability to Manage Drug Costs
Other stakeholders have proposed policies that would limit the ability of employers and purchasers to manage their drug costs including banning step therapy and generic substitution. These policies would further drive up health costs for purchasers and families, and have no basis in clinical efficacy. EmployersRx will strongly oppose these policies which strip employers and purchasers of their already limited ability to manage their drug costs
State Policy Solutions
April 14th, 2021
Effective markets require healthy competition and transparent information on cost and quality. Unfortunately, these conditions don’t exist in all health care markets. Entrenched interests feed off market failures and use their political muscle to keep the broken status quo in place. If we’re going to rely on competitive market forces to keep prices reasonable, government must step in to make sure that markets are working the way they should. In some areas, however, the market is fundamentally broken, and it is nearly impossible to address costs through competition. In these situations, government needs to step in to limit prices.
As the leading voice of large national employer health care purchasers on public policy, PBGH has a track record of advocating for a market environment of healthy competition and successfully influencing both state and federal policy to enhance, among other priorities, value-based purchasing and the restriction of anti-competitive practices in order to improve affordability and quality.