Federal Policy Solutions
April 14th, 2021
Effective markets require healthy competition and transparent information on cost and quality. Unfortunately, these conditions don’t exist in all health care markets. Entrenched interests feed off market failures and use their political muscle to keep the broken status quo in place. If we’re going to rely on competitive market forces to keep prices reasonable, government must step in to make sure that markets are working the way they should. In some areas, however, the market is fundamentally broken, and it is nearly impossible to address costs through competition. In these situations, government needs to step in to limit prices.
As the leading voice of large national employer health care purchasers on public policy, PBGH has a track record of advocating for a market environment of healthy competition and successfully influencing both state and federal policy to enhance, among other priorities, value-based purchasing and the restriction of anti-competitive practices in order to improve affordability and quality.
Sutter Health
April 14th, 2021
PBGH brought employers and unions together with California’s Attorney General to successfully file a class action suit against Sutter Health’s use of market power and monopolistic business practices that cost employers and employees. This has been a 10-year effort by PBGH that was settled December 2019. Most eligible California employers and unions have now received an initial settlement payout.
Details of the Landmark Settlement
The settlement: $575 million
10-Year injunctive relief: Potential greater dollar value to employers and purchasers:
- Limit chargemaster increases
- Reduce surprise billing
- Prevent all-or-nothing contracting practices
The Price Employers Paid
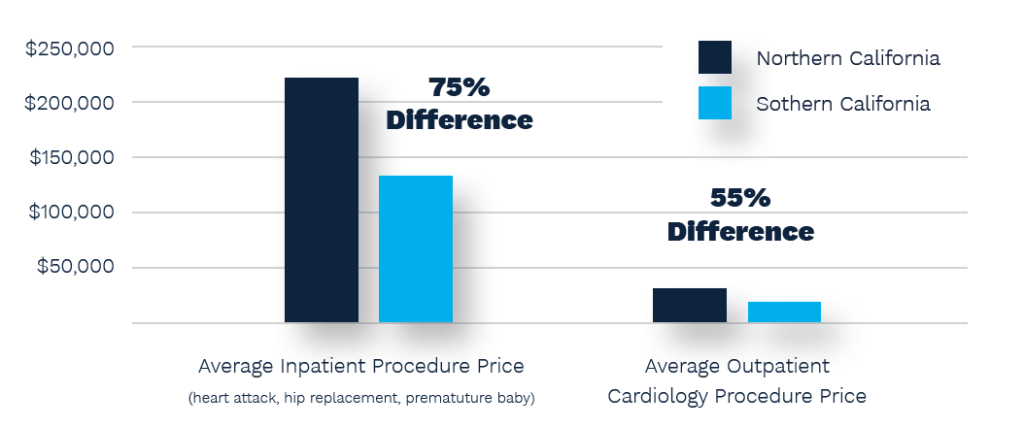
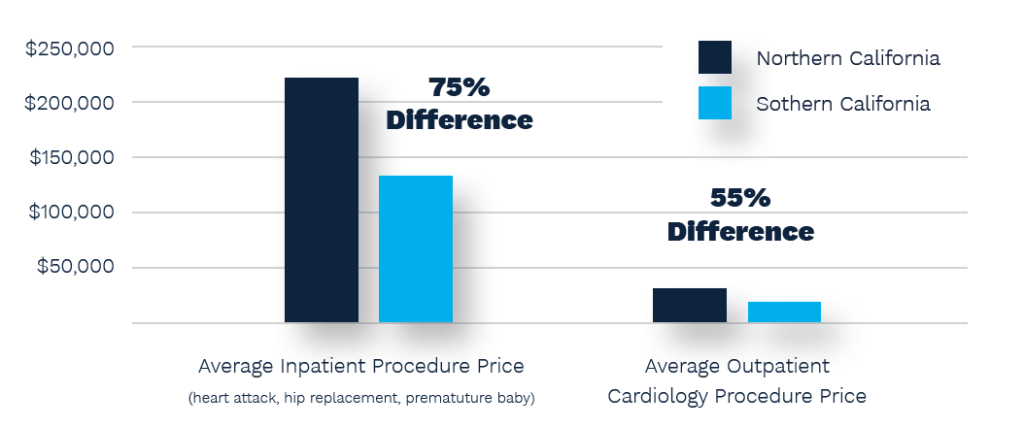
Sutter’s profit from commercially insured patients averaged over $1.5 billion annually, representing a 43% margin more than the last decade. Average hospital inpatient procedures in Northern California cost $223,278 compared to $131,586 in the South.
The Windfall for Employers
California-based companies, government entities and labor trusts will receive a payout based on past medical claims overpayments to Sutter Health.
Payouts vary based on the disparity between excess Sutter rates compared to the geographic community and the dates claims were incurred.
Hospital Consolidation Impact on Price
Negotiating Alliance Services
March 12th, 2021
Large employers and purchasers have long had to rely on intermediaries with conflicting business interests to procure health services and benefits programs. Too often this leads to opaque supplier contracts that add wasteful and unsustainable costs for those paying the bills.
Building on a long history of providing purchasers analytic and technical expertise, PBGH engages with members eager to upend the status quo and bypass traditional actors in the health care ecosystem for independent partners. We support vendor evaluation and selection and bring together subject matter experts and purchasers to share procurement experiences that inform contracting arrangements designed to deliver better care, often at significantly lower cost.
Past work on behalf of large employers and other health care purchasers includes:
- The PBGH Negotiating Alliance, through which purchasers leveraged their collective volume to improve quality and affordability in joint California HMO negotiations for nearly 20 years. Negotiating Alliance initiatives have shaped contracting that has rewarded better provider networks, responded to the needs of the chronically ill and created tools that support consumers’ informed decision-making. Our efforts have resulted in hundreds of millions in cost savings, while improving the care and experience of consumers.
- Health plan assessment and value-based contracting using the eValue8 health plan RFI, adoption of industry-leading performance guarantees and premium benchmarking with risk-adjusted claims analytics.
- Pharmacy benefit procurement through joint purchasing, custom formulary design and industry-leading contract terms to promote rebate transparency, aligned incentives and waste reduction.
- Launched Retiree Health Access with HealthCare Policy Roundtable as a group and individual retiree solution for large employers.
- Assessment of disease management and wellness programs offered by health plans and standalone vendors. PBGH designed pilot programs and audited care coordination and high-cost case management, and the development of standardized contract language and performance guarantees for clinical quality and patient experience.
- Support for data warehouse and analytics vendor procurement processes for diverse organizations, including Health Transformation Alliance and Covered California.
- Evaluation of private exchange products.
- Assessment of EAP and digital mental health vendors.
Primary Care Payment Reform Workgroup
February 9th, 2021
The PBGH Primary Care Payment Reform Work Group is an employer/purchaser-led initiative to remove barriers to better health outcomes by shifting away from traditional fee-for-service payment and toward alternative payment models that support the provision of “advanced primary care.” This includes payment that enable team-based care, integration with mental health, robust virtual access and other characteristics of advanced care.
The workgroup’s objectives include:
- Building purchaser consensus for new payment models that support and enable advanced primary care.
- Identifying and endorsing a core set of measures to reflect the better patient outcomes and experience of advanced primary care.
- Developing sample contract language to support advanced primary care payment.
- Engaging purchasers to monitor progress toward payment models that enable advanced primary care practice.
- Facilitating alignment with other regional primary care transformation efforts.
- Considering options for working more directly with provider organizations.
Employers Centers of Excellence Network
January 22nd, 2021
The Employers Centers of Excellence Network (ECEN) provides employees access to demonstrated high-quality care for elective surgeries at meticulously selected Centers of Excellence (CoE) across the United States. Through the ECEN, patients receive care at little or no cost, and their employers gain predictable health care costs and downstream savings.
The ECEN was established based on and inspired by PBGH members’ interest in supporting value-based purchasing and the program aligns with PBGH’s ongoing mission to be a change agent creating increased value in the health care system through purchaser collaboration, innovation and action and through the spread of best practices. In early 2013, a group of eight forward-thinking self-insured employers came together to help PBGH design the ECEN program with the aim of selecting hospitals and surgeons throughout the nation for hip and knee replacements. The ECEN later expanded to offer spine and bariatric procedures and certain oncology services.
By encouraging employees to utilize carefully selected, high-quality hospitals and surgeons for these procedures, the ECEN reduced variation in quality and cost and increased the likelihood of optimal patient outcomes. Quality improvements and decreased costs resulted from improved professional care coordination, team attention to evidence-based guidelines, better discharge planning to avoid preventable readmissions, increased uniformity of practice and measurement and feedback of patient outcomes.
Since its launch, the ECEN received very positive reviews from employers and patients alike, with 98% of patients recommending the program.
Multi-Payer Claims Database
January 22nd, 2021
Imagine trying to purchase a car without knowing anything about how good it is or what it will cost. That’s the situation consumers face when choosing a doctor.
Consumers simply don’t have the information they need to pick a doctor based on measurable quality or the expected cost of care. Instead, they usually select physicians based on convenience or referrals. In addition, while most physicians sincerely want to give their patients high-quality care, they don’t know how they stack up to each other and are not competing to attract patients.
PBGH, under a contract with the California Healthcare Performance Information System (CHPI), administered what at the time was the only Multi-Payer Claims Database (MPCD) in operation in California. It consisted of claims from the state’s three largest health plans and the Medicare fee-for-service program.
In all, CHPI aggregated administrative claims and eligibility data for approximately 12 million lives across California to create physician performance ratings.
MPCD Program Summary
Making Wise Health Care Choices Together
January 22nd, 2021
PBGH in collaboration with Consumer Reports developed the Choosing Wisely microsite.
Choosing Wisely resources encourage conversations between health care providers and consumers about overuse or misuse of medical tests, treatments and procedures that may provide little benefit and, in some cases, may cause harm. PBGH also worked with Consumer Reports to help educate consumers through a Choosing Wisely Employer Toolkit for companies to educate their employees about the overuse of health care resources.
Consumer-Purchaser Alliance
January 22nd, 2021
The Consumer-Purchaser Alliance was created to ensure that the voices of consumers and purchasers influence the improvement and redesign of the health care system. Our focus has been on value: better health outcomes and patient experience, at the lowest possible total cost of care. We believe that the health care system works best when consumers and purchasers have the information they need to make meaningful choices that reflect their needs and priorities. Our mission was to strengthen the voice of consumers and purchasers in the quest for higher quality, more affordable health care.
Underlying our mission is the core belief that provider payment models and performance measures are critical tools to drive change in the health system. Traditional payment models have rewarded volume of services rather than value. Until payment models are changed to reward better quality care, patient experience, appropriate use and efficiency, our health care system is unlikely to deliver improved value.
In order to reward value, of course, it is essential to measure it. Traditional measures have focused on the process of care rather than health outcomes, and they have seldom incorporated patient-generated data. In addition to their use in payment models, performance measures are essential for consumers and purchasers in making choices about doctors, hospitals, treatment plans, benefit designs and health plans. Until performance measures are improved to include clinical outcomes, patient-reported outcomes, patient experience and total cost of care, our health care system is unlikely to improve.
Co-chaired by the National Partnership for Women & Families (NPWF) and Pacific Business Group on Health (PBGH), the Consumer-Purchaser Alliance consisted of over 50 consumer, labor and purchaser organizations (See ‘The Legacy of Consumer-Purchaser Alliance from 2003-2018: Accomplishments and Lessons Learned’ below for a list of participants). The project was funded by the Robert Wood Johnson Foundation from 2003 to 2018.
Legacy Products
For 15 years, the Alliance catalyzed change in the way the health care system addressed the needs of those that receive and pay for care by creating an infrastructure that allowed consumers and purchasers to exert influence on the policy landscape. The unconventional collaboration of consumers and purchasers disrupted the power dynamics in health care policymaking, and their combined efforts produced results greater than their individual contributions alone. The history of the Alliance, including lessons learned and key achievements, is encapsulated in: The Legacy of the Consumer-Purchaser Alliance from 2003-2018: Accomplishments and Lessons Learned
The Consumer-Purchaser Alliance also left behind a set of products to inform and assist consumer and purchaser organizations that want to shape the future direction of our health care system.
- The principles for provider payment models and criteria for performance measures are intended to help consumer and purchaser organizations and representatives engage with other stakeholders and policymakers in key decision forums.
Principles for Payment Models: Advancing Consumer & Purchaser Priorities
10 Criteria for Meaningful and Usable Measures of Performance
- The patient-reported outcomes toolkit is intended to support consumer and purchaser advocacy of high-value patient-reported outcome measures (PROMs) and patient-reported outcome performance measures (PRO-PMs) in clinical practice, for consumer choice and for provider payment. The toolkit consists of an Advocacy Guide and a Selection Guide. The Advocacy Guide describes C-P Alliance’s proven advocacy strategies for advancing widespread adoption and use of PROMs and PRO-PMs. The Selection Guide supports advocates in making specific PROM/PRO-PM recommendations for six high-impact clinical conditions (asthma, depression, coronary artery disease, heart failure, hip replacement and knee replacement) by allowing advocates to quickly understand which PRO tools (of the hundreds that exist) are 1) ready for use in clinical practice and 2) meet the needs of consumers and purchasers
Promoting the Use of Patient-Reported Outcome Measures: Practical Tools for Consumers-and Purchasers
Historical Documents: Public Comments, Issue Briefs, etc.
The following are a selection of high-impact public comment letters and other documents that chronicle consumer and purchaser perspectives on key issues and programs
Key Issues
Federal Programs
Center for Medicare & Medicaid Innovation Center (CMMI)
Quality Payment Program (QPP)
Inpatient Prospective Payment System (IPPS)
Episode Payment Models
Meaningful Use & Health Information Technology
California Joint Replacement Registry (CJRR)
January 21st, 2021
The California Joint Replacement Registry (CJRR), collected and shared data to provide credible feedback to orthopedic surgeons, hospitals and patients about their treatment decisions, quality of care and patient outcomes. Operated by PBGH for several years, CJRR was created to meet the need for comprehensive, scientific assessment of devices, treatment protocols, surgical approaches and patient factors influencing the results of hip and knee replacement surgeries for the State of California. In March 2015, the CJRR was transitioned to the American Joint Replacement Registry (AJRR).
The CJRR is one of only two registries in the U.S. that collects and incorporates clinical information along with patient-reported outcome measures (PROMs), such as patients’ overall health, pain and energy before and after their joint replacement procedures. CJRR has published hospital performance information online and in annual reports in an effort to drive care improvement and support emerging payment and health care delivery models. With the help of CJRR, providers will be assessed based on their patient outcomes, while their payments and inclusion in provider networks will be based on performance. The long-term goals are to improve treatment decisions and care delivery for patients receiving joint replacements.
CJRR has 41 participating institutions and 225 participating surgeons in its registry. Though the project has transitioned to another entity, PBGH staff continue to contribute to the project’s advisory committee, the California Data Use Group. For more information, please visit http://www.ajrr.net/cjrr.
Tackling High Costs
January 11th, 2021
American consumers pay more for health care than people in any other country. Purchasers of health care in the private insurance market pay most of all. PBGH seeks to uproot the economic distortions in the nation’s health care payment and delivery system to ensure that health care is affordable and accessible to everyone in the country. We support policies to improve competition and transparency, and — where necessary — give regulators the ability to ensure fair and reasonable prices for health care.