Behavioral Health
October 25th, 2024
Behavioral health is an essential component of high-quality, patient-centered care, as mental health and substance use concerns directly impact patients’ overall well-being and physical health outcomes. Through its behavioral health integration programs, CQC is helping primary care providers address these needs alongside physical health, fortifying primary care to deliver equitable, whole-person care. Although three out of four primary care visits in California include a mental health concern, many patients are unable to access the treatment they need due to provider shortages, fragmented care and limited screening. Data shows that only 33% of patients are asked about mental health symptoms during medical visits, and even fewer receive the treatment they need.
CQC’s Behavioral Health Integration Initiative is bridging these gaps through evidence-based models that enhance screening, expand access to care and equip primary care teams to meet the comprehensive needs of their patients. Current programs incentivize screenings, offer targeted training and leverage patient-reported data to address critical access issues across the state. By aligning incentives and integrating behavioral health services, CQC is creating sustainable pathways to improve outcomes and ensure that underserved populations receive the mental health care they deserve.
Advanced Primary Care
October 25th, 2024
For over a decade, CQC has led initiatives to transform primary care into a foundation for healthier, cost-effective outcomes across California. Through its work with diverse stakeholders — including health plans, purchasers and providers — CQC has pioneered the development of the Advanced Primary Care model, which places patients at the center of every interaction and defines high-quality care through patient-centered, results-oriented measures.
By establishing shared attributes and measures, CQC enables payers, providers and health care purchasers to identify, incentivize and expand high-performing practices. Building on a statewide practice transformation initiative funded by the Centers for Medicare and Medicaid Services, CQC’s definition of Advanced Primary Care now serves as a blueprint for quality improvement nationwide. Current programs and initiatives demonstrate how coordinated efforts can standardize high-value primary care, aligning financial incentives to improve access, patient outcomes and cost efficiency.
Publications
October 24th, 2024
Consulting & Coaching
October 23rd, 2024
CQC leverages extensive consulting and coaching expertise in health care quality improvement, focusing on key areas designed to elevate care and operational efficiency. Our services are tailored to meet the distinct needs of practices and health care organizations, helping them enhance operational capabilities and align strategies with industry standards and policies.
Intensive Outpatient Care Program
September 4th, 2024
Dates Active: 2012-2015
The Intensive Outpatient Care Program (IOCP) was a three-year initiative led by the California Quality Collaborative from 2012 to 2015 through a CMS Innovation Center grant. The program supported 23 participating provider organizations serving over 15,000 Medicare beneficiaries across Arizona, California, Idaho, Nevada, and Washington in adopting a patient-centered, team-based care model to manage high-risk, medically complex patients. IOCP focused on improving clinical outcomes, enhancing patient experience, and reducing the utilization of high-cost care services such as emergency department visits and hospitalizations. The program enrolled over 9,500 patients, particularly targeting those whose outcomes could be significantly improved through enhanced care coordination.
Program Overview
IOCP provided a comprehensive framework for integrating intensive outpatient care into participating healthcare organizations’ existing services. Key elements of the program included:
- Multidisciplinary Team-Based Approach. Central to the IOCP model was a care coordinator who served as the primary link between patients and their care teams, including primary care, specialty services and community resources.
- Comprehensive Care Coordination. The program emphasized coordination of medical, behavioral and psychosocial care tailored to the needs of patients with chronic illnesses and multiple comorbidities.
- Patient-Centered Care Planning. Care coordinators worked with patients to develop individualized care plans that aligned with their personal health goals and needs.
- Support for Self-Management. Patients were provided with tools and resources to manage their conditions effectively, reducing dependency on emergency and inpatient services.
Participant Support
IOCP participants received:
- Funding and Grants. Financial support to implement and sustain the intensive outpatient care model.
- Training and Curriculum. Access to a comprehensive training curriculum focusing on patient-centered care, care coordination and self-management strategies.
- Peer Learning Opportunities. Regular learning sessions and workshops to share insights, strategies and best practices among peers.
- Technical Assistance. Ongoing support from CQC and its partners, including expertise in care model design, data analytics and quality improvement.
Program Outcomes
IOCP achieved significant improvements in both patient outcomes and health care utilization:
- Reduction in Depression Symptoms. The program reported a 33% improvement in average PHQ-9 scores among participants, indicating better management of depression.
- Reduction in Cost of Care. 21% reduction in cost of care for high-risk patients enrolled for at least nine months.
- Increased Patient Activation. 3.6% patient engagement increase of patients advancing to a higher level of activation.
- Health Status Improvement. Participants showed a 3.4% increase in mental health composite scores and a 4.1% increase in physical health composite scores, according to the Health Status Survey (VR-12) results.
Funding
IOCP was made possible by the generous support of the Centers for Medicare & Medicaid Services.
Cal-IN Peer Group
June 14th, 2024
In partnership with the Collaborative Family Healthcare Association, the California Quality Collaborative (CQC) is hosting quarterly virtual peer group meetings for individuals working to integrate behavioral health care into the primary care setting in California.
Participant Benefits
Participants of the Cal-In Peer Group will have the opportunity to:
- Connect with peers within California’s behavioral health integration space
- Share behavioral health integration experience, including challenges and successes
- Brainstorm and commit to potential future collaborations
Meeting Dates
The Cal-In Peer Group 2025 virtual meeting dates are:
- Wednesday, March 19 | 12 – 1 p.m. PT
- Wednesday, June 18 | 12 – 1 p.m. PT
- Wednesday, September 24 | 12 – 1 p.m. PT
- Wednesday, December 3 | 12 – 1 p.m. PT
How to Join
Those interested in participating should complete this interest form and CQC will follow up with you soon.
California Medicare Collaborative
May 15th, 2024
California’s over-65 population is diversifying and growing faster than any other age group. By 2030, it will represent a quarter of the population, which means addressing their unique health and long-term care needs will become critical, requiring creative solutioning for the delivery ecosystem. Medicare beneficiaries tend to have chronic conditions, need a variety of providers and services and may experience daily living challenges, leading to difficulty navigating a complex system of medical and nonmedical services when seeking to live a healthy, safe life at home. Medicare-only individuals are often forgotten in their struggles to finance and access the services and support they need across the health care, behavioral health, and long term services and supports delivery systems.
To address this need, the California Quality Collaborative (CQC), The SCAN Foundation, Archstone Foundation, Gary and Mary West Foundation and Department of Health Care Services Office of Medicare Innovation and Integration, will launch the California Medicare Collaborative, a one-year stakeholder alignment effort beginning in March 2024, dedicated to improving care across the spectrum of Medicare enrollees, including duals, non-duals and those in traditional Medicare and Medicare Advantage programs.
Goals and Areas of Focus
The collaborative will focus on the following four areas:
- Cognitive and behavioral health
- Chronic illness management and care coordination
- Support consumer choice in a confusing market
- Access, equity and disparities in care
CQC’s goal is to gain consensus within each focus area by the end of 2024 on opportunities for action that can be achieved through alignment and partnerships among California delivery system stakeholders and to secure commitment from these stakeholders to support implementation of those action steps following the close of the collaborative.
Participants
CQC, along with the Department of Health Care Services’ Office of Medicare Innovation and Integration (OMII) and our funders, is seeking to involve a wide range of stakeholders. This diverse representation will ensure that a range of organizational perspectives influencing Medicare care delivery in California are considered. Participants will have the opportunity to forge valuable connections with peers and actively contribute to shaping the future direction and strategy of California’s Medicare system.
Support
This program is made possible thanks to the support of The SCAN Foundation, the Archstone Foundation and the Gary and Mary West Foundation, in collaboration with the Department of Health Care Services Office of Medicare Innovation and Integration.
Comprehensive Maternity Care Workgroup
May 6th, 2024
The United States has the highest rate of maternal mortality among wealthy nations. Moreover, women of color are more likely than white women to die from complications of childbirth, and access to maternity care is decreasing as maternity care deserts – counties with limited or no maternity care – become increasingly common. Employers pay for more than half of the births in the U.S. and can play a significant role in impacting maternal and infant health outcomes on behalf of workers and their family members.
PBGH’s Comprehensive Maternity Care Workgroup, launched in summer 2022 and co-chaired by Qualcomm Incorporated and Walmart, brings together employers and public purchasers to achieve high-quality, affordable and equitable health care for mothers and babies.
The workgroup, in partnership with other stakeholders and subject-matter experts, has developed tools to advance that goal, including a shared standard to define Comprehensive Maternity Care, a purchaser Priority Maternity Measure Set to ensure accountability and transparency and the PBGH Comprehensive Maternity Care Common Purchasing Agreement, which provides benefit design and purchasing recommendations for employers and public purchasers, health plans and providers. These tools are intended to help ensure public and private purchasers are purchasing accessible, high quality and equitable maternal care for their workers and family members.
For questions regarding PBGH’s maternal health and birth equity work or opportunities to partner, please contact Randa Deaton at rdeaton@pbgh.org.
Collective BHI Solutions
April 17th, 2024
Integrating behavioral health into primary care ensures providers deliver timely, patient-centered, comprehensive whole-person care while expanding access to behavioral health services, improving patient outcomes, enhancing care team satisfaction and reducing total cost of care. CQC’s Collective BHI Solutions consist of alignment efforts that bring together stakeholders across California’s delivery system, including purchasers, health plans and provider organizations, to address specific pain points such as defining behavioral health integration and behavioral health integration financing.
Behavioral Health Integration Payer Workgroup (2025)
In 2025, CQC will be convening a workgroup supporting commercial health plans to:
- Collaborate with peers and subject matter experts to facilitate BHI implementation for plans and providers
- Co-design documents to help prepare plans and providers for BHI implementation:
- BHI Policy/FAQ for plans
- BHI implementation guide for providers
- BHI data request process
- Create a network of health plan leaders ready to support BHI
Workgroup documents will be shared publicly.
Participating organizations: Aetna, Blue Shield of California, HealthNet, Sharp Health Plan, United with Optum, Western Health Advantage with Optum
Multistakeholder Alignment for BHI (2025)
CQC will conduct interviews with four states experienced in multistakeholder alignment for BHI. Additionally, CQC will draft a proposed definition of behavioral health integration in primary care through a consensus process with various California stakeholders. Interview findings will be synthesized into recommendations for California in Q4 2025.
Behavioral Health Integration – Financing Opportunities (2024)
In 2024, CQC conducted a state-wide landscape assessment project to identify, synthesize and communicate successful practices to ensure sustainable payment for behavioral health integration into primary care. CQC interviewed key stakeholders, including health plans and provider organizations, addressing related contracts, claims, credentialing and strategic planning, summarized in our Sustainable Behavioral Health Integration Financing: Successful Practices and Opportunities issue brief. The paper identifies practices that facilitate sustainable payment for behavioral health integration (BHI) into primary care in commercial settings for providers, payers, purchasers and regulators.
Support
Behavioral Health Integration Financing is possible thanks to the generous support of Blue Shield California Industry Initiatives.
Behavioral Health Integration – Children and Youth Collaborative Learning Exchange
March 8th, 2024
Launched October 2024, the Behavioral Health Integration – Children and Youth Collaborative Learning Exchange is a nine-month learning collaborative that brings together organizations experienced in integrating behavioral health services into primary care for children and youth.
Collaborative Objectives
By July 2025, the collaborative aims to have improved behavioral health integration for children and youth served by leading provider organizations by:
- Showcasing successful practices and highlighting solutions through a vibrant network of peer organizations
- Sprouting adoption of new solutions addressing real-world challenges that improve the delivery of pediatric and adolescent integrated behavioral health care
- Sharing best practices through a public toolkit that synthesizes collaborative participants’ recommendations, experience and contributions to the field
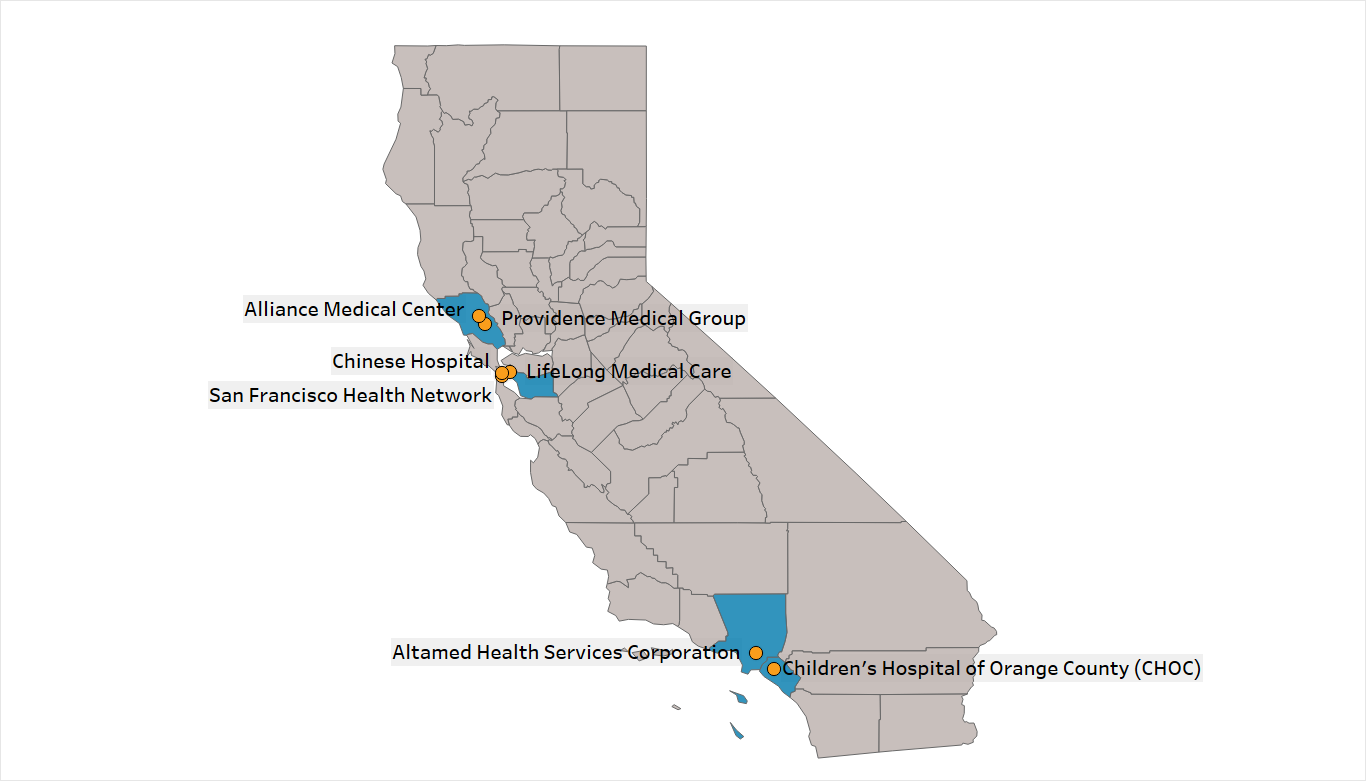
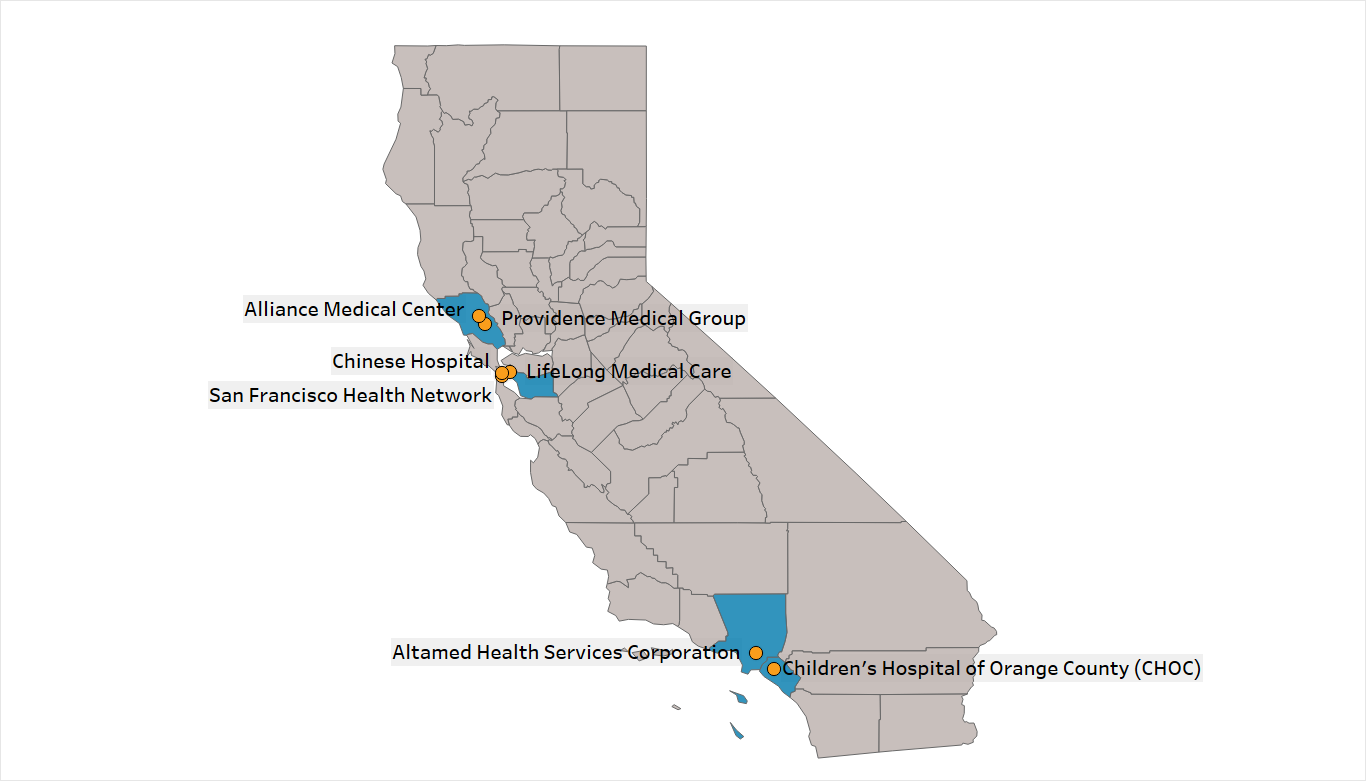
Participating Organizations
Organizations participating in the collaborative will receive:
- Funding of up to $7,500 over the course of the collaborative to support the advancement of behavioral health integration
- Facilitated monthly peer meetings that promote sharing and learning from a dynamic network of peer health care organizations
Technical Assistance Partner
CQC is partnering with Rady Children’s Health for the Behavioral Health Integration – Children and Youth Collaborative Learning Exchange technical assistance program. Rady Children’s Health is the largest provider of comprehensive pediatric medical services in the San Diego region and a leader in integrated behavioral health. The hospital launched a primary care behavioral/mental health integration program in 2020 that provides evidence-based mental health care through embedding mental health clinicians in pediatric primary care practices for easy, same-day access.
Support
CQC’s Behavioral Health Integration Initiative is made possible thanks to the generous support of the Centene Corporation.