Payment Model Demonstration Project Technical Assistance
January 19th, 2024
Providers contracting for any version of the California Advanced Primary Care Initiative’s common value-based payment model through the Payment Model Demonstration Project will engage in technical assistance to support performance improvement. Technical assistance services are provided by the California Quality Collaborative (CQC).
Technical assistance includes evidence-based support through a combination of on-demand virtual learning resources and personalized guidance from an improvement coach who interacts with practices via regular coaching sessions and remains available for questions and support throughout the project. Improvement coaches partner with practices to understand needs and opportunities, set goals, guide improvement efforts and track progress. In addition, participating practices will convene together every quarter to exchange learnings, provide peer support for overcoming challenges and celebrate achievements.
Curriculum
The foundation of the technical assistance program focuses on concepts from evidence-based frameworks and best practices, including:
- Model for Improvement
A widely used framework from the Institute for Healthcare Improvement for developing, testing and implementing changes leading to improvement.
- 10 Building Blocks of High-Performing Primary Care
A roadmap to identify foundational capabilities and implement building blocks, that include practice-level advanced primary care capabilities like engaged leadership, data-driven improvement, team-based care and population management. CQC has developed webinars on the 10 Building Blocks of Primary Care.
- Practice Transformation Initiative
An assessment, change package and curriculum developed by CQC and used across more than 2,000 California primary care practices to guide transformation efforts and improve care and health outcomes.
Participating Practices
Additional Support and Resources
In addition to learning practice-level change concepts, participants will have access to skill-building trainings such as improvement coaching, motivational interviewing and patient and family engagement techniques.
Advanced Primary Care Measurement Pilot
January 17th, 2024
Dates Active: 2022-2023
Together with IHA, PBGH brought together four large health care purchasers in California to pilot CQC’s set of practice-level performance measures that emphasize patient experience and outcomes. The Advanced Primary Care Measurement Pilot began in January 2022, and participating purchasers include Covered California, California Public Employees’ Retirement System (CalPERS), eBay and San Francisco Health Services System.
The information gained in the pilot can be used by purchasers and health plans to better connect patients to practices delivering the best primary care in the market and incentivize improvement for other providers, increasing the availability of Advanced Primary Care.
Payment Model Demonstration Project
January 17th, 2024
The Payment Model Demonstration Project will test a common value-based payment model with approximately 30 independent practices in California to strengthen primary care delivery. The overarching goal of the demonstration project is to provide additional resources for primary care providers, equipping them to deliver high-quality patient care and achieve better outcomes. These resources include helping to boost revenue, providing technical assistance and delivering data exchange and insights. Due to the variety of payers that practices contract with, implementing payment changes collectively has the potential to yield greater positive impact compared to individual plan-driven efforts.
As the next phase of the California Advanced Primary Care Initiative, the demonstration project is a collaboration of PBGH’s California Quality Collaborative (CQC) and the Integrated Healthcare Association (IHA), as well as three participating health plans – Aetna, Blue Shield of California and Health Net – beginning October 1, 2024 and ending December 31, 2025.
Barriers for Primary Care Practices
Primary care is the backbone of any high-performing health care delivery system, but it has been chronically underfunded, receiving approximately 4-7% of health care dollars while about 55% of health care visits take place in primary care settings.
The many barriers to the delivery of advanced primary care were underscored by pandemic burnout experienced by primary care providers. Small independent primary care practices, the primary focus of this demonstration project, are particularly affected by these barriers, which include misaligned payer incentives, minimal integration with other elements of care and the lack of necessary infrastructure, technology and workforce.
Common Value-Based Payment Model
Through the payment demonstration project, health plans will offer two similar versions of a value-based payment model. Practices may be paid under one or both depending on which health plans they contract with. Both value-based payment models invest more revenue into the practice and reward improvement and strong performance on the Advanced Primary Care Measure Set.
Hybrid Model:
- Monthly per member per month (capitated) payment
- Volume-based payment for specific pre-defined services (focusing on preventive care)
- Population health management payment to support practice improvements that will deliver better outcomes
- Incentives for strong performance on a common set of outcomes measures.
Fee-for-Service “Plus”:
- Volume-based payment for all services
- Population health management payment to support practice improvements that will deliver better outcomes
- Incentives for strong performance on a common set of outcomes measures.
Participating Practices
Support for Practices on How Best to Use the New Revenue
Focused support will be available to participating practices through a technical assistance program. The support will include regular one-on-one coaching to advise care teams on how to optimize their additional revenue for practice transformation.
Practices will have access to a common reporting platform to assess measure performance and progress across all participating health plans to reduce administrative burden. Plans will be trained on the platform as will the technical assistance coaches to manage troubleshooting and potential issues.
How Success Will Be Measured
Quantitative success will include return on investment for plans based on relative improvement on several key clinical and utilization measures, overall improvement on the Advanced Primary Care Measure Set for each practice and comparisons across practices, including the proportion of patients paid under each version of the value-based payment model and other variables.
Qualitative information on practice experience, engagement and impact is collected by technical assistance coaches to assess trends and make adjustments for future scaling of this multi-payer work. Information on the health plans’ experiences with multi-payer partnership is also collected with an eye toward learnings, improvement and future scaling.
View our complete introductory video series for an inside look at the Payment Model Demonstration Project
California Data Exchange Framework
April 18th, 2023
Rapid data exchange within the health care delivery system is integral to achieving equitable, patient-centered care for all Californians. The California Quality Collaborative (CQC) supports the California Health and Human Services Agency’s Data Exchange Framework (DxF), the first-ever statewide data sharing agreement, because it will accelerate and expand the exchange of health information among health care entities, government agencies and social service programs. Find the most up-to-date resources and events on the Connecting For Better Health Hub.
DxF implementation is a multi-year process that has involved extensive stakeholder engagement. With stakeholders, the California Health and Human Services Agency’s Center for Data Insights and Innovation (CDII) has published a data sharing agreement and associated policies and procedures that explain the “rules of the road” for data sharing in California, and these materials will be continuously updated as needs change and standards evolve. There is also a mandate that certain specified entities sign the DSA by January 31, 2023 and begin sharing data by January 31, 2024.
CQC is part of a multi-association collaborative promoting participation in the DxF. Get more information, including timelines and updates, here.
Additional information is also available from the California Medical Association.
Behavioral Health Integration Initiative
January 4th, 2023
Meeting patients’ mental health needs and considering social impacts on their health are fundamental to providing comprehensive, patient-centered and high-quality care. However, the lack of improvement in screening and care access demonstrates the need for greater investment to support primary care practices in efforts to integrate behavioral health services.
CQC will work on a Behavioral Health Integration Initiative from 2022 through 2027 that will accelerate integration efforts by small and independent primary care practices throughout the state. The initiative aims to improve screening, diagnosis and treatment of patients’ mild-to-moderate behavioral health needs, like depression, anxiety and substance use disorder.
This includes:
- Direct technical assistance and funding to primary care practices engaged in improvement efforts through the CalHIVE Behavioral Health Integration Improvement Collaborative
- Better understanding patient perspectives of their behavioral health needs, access to care and treatment through expanded surveying
- Development of common standards for patient privacy, consent and data sharing among payers and providers to reduce administrative burden to integrating care
Support
CQC’s Behavioral Health Integration Initiative is possible thanks to the generous support of Centene Corporation, California Health Care Foundation and Blue Shield California Industry Initiatives.
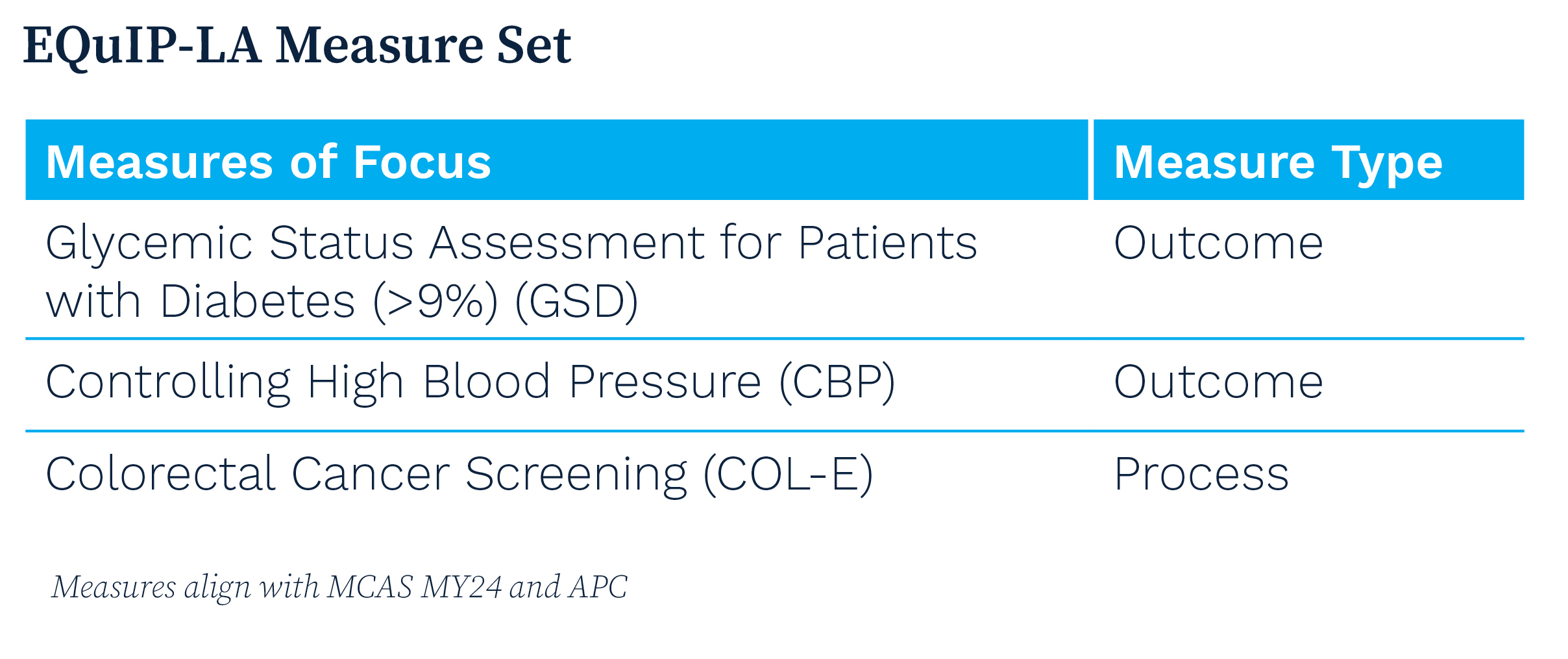
Equity and Quality at Independent Practices in LA County
December 5th, 2022
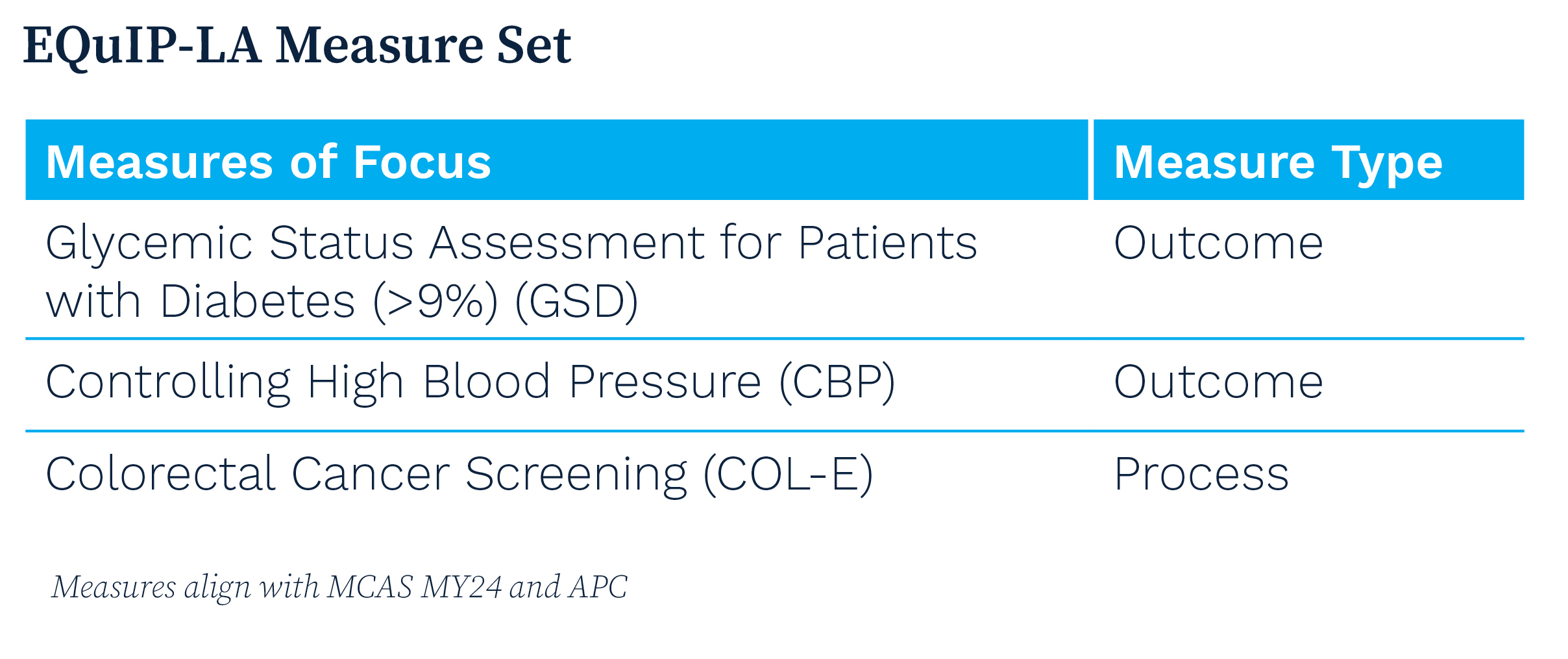
Launched in 2023, Equity and Quality at Independent Practices in LA County (EQuIP-LA) was a two-year improvement collaborative led by the California Quality Collaborative (CQC) dedicated to reducing disparities of care experienced by Medi-Cal enrollees of color.
EQuIP-LA is supporting participating organizations by:
- Building their capacity and that of community-based practice coaches to implement an equity-centered approach to quality improvement
- Incorporating patients’ lived experiences into the co-design of the collaborative’s curriculum
- Designing and implementing interventions to address disparities of care related to chronic disease management and preventative screening, focusing on diabetes, hypertension and colorectal cancer screening
- Advancing the practice capabilities necessary for delivering advanced primary care
Participating Organizations
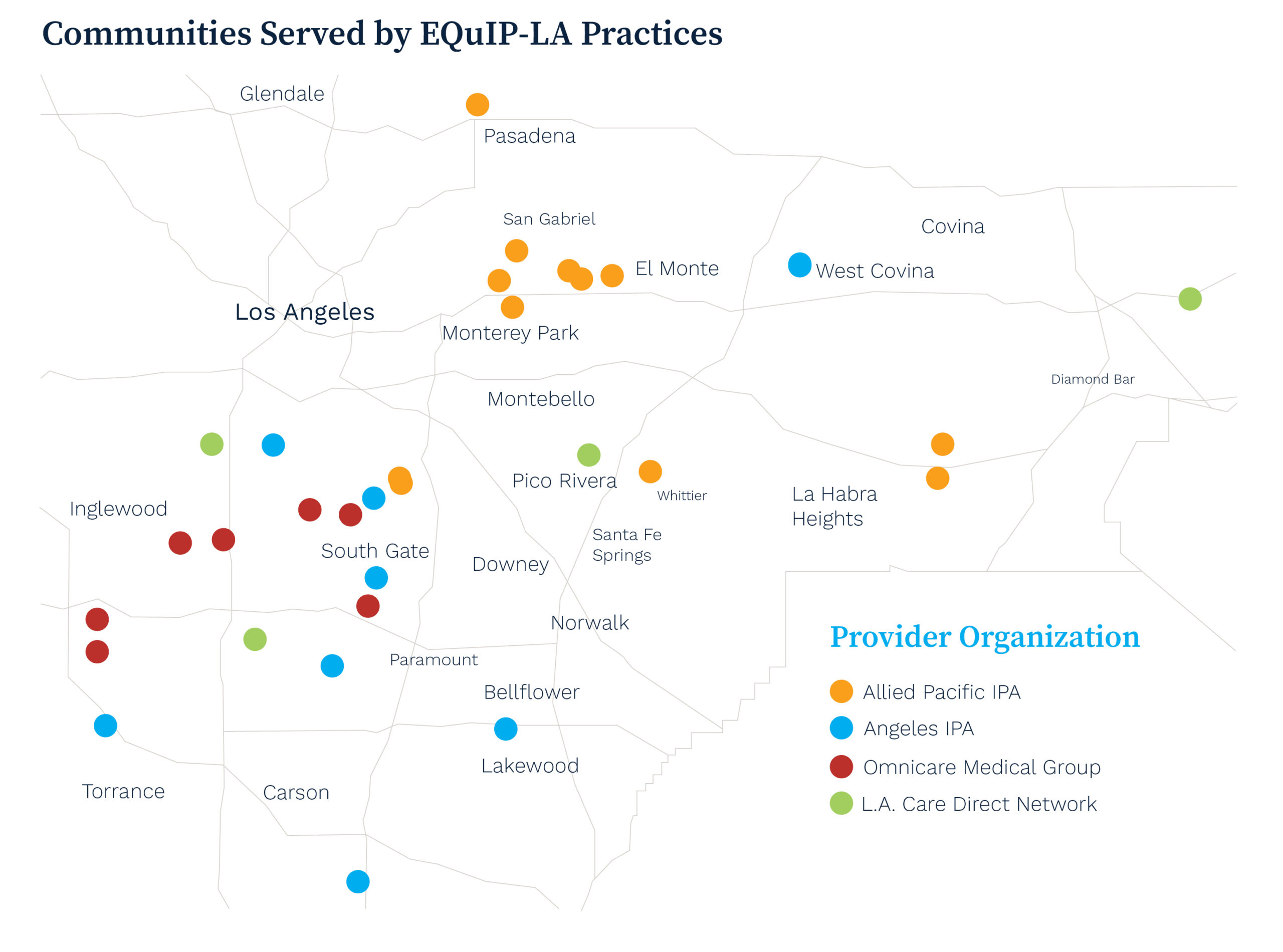
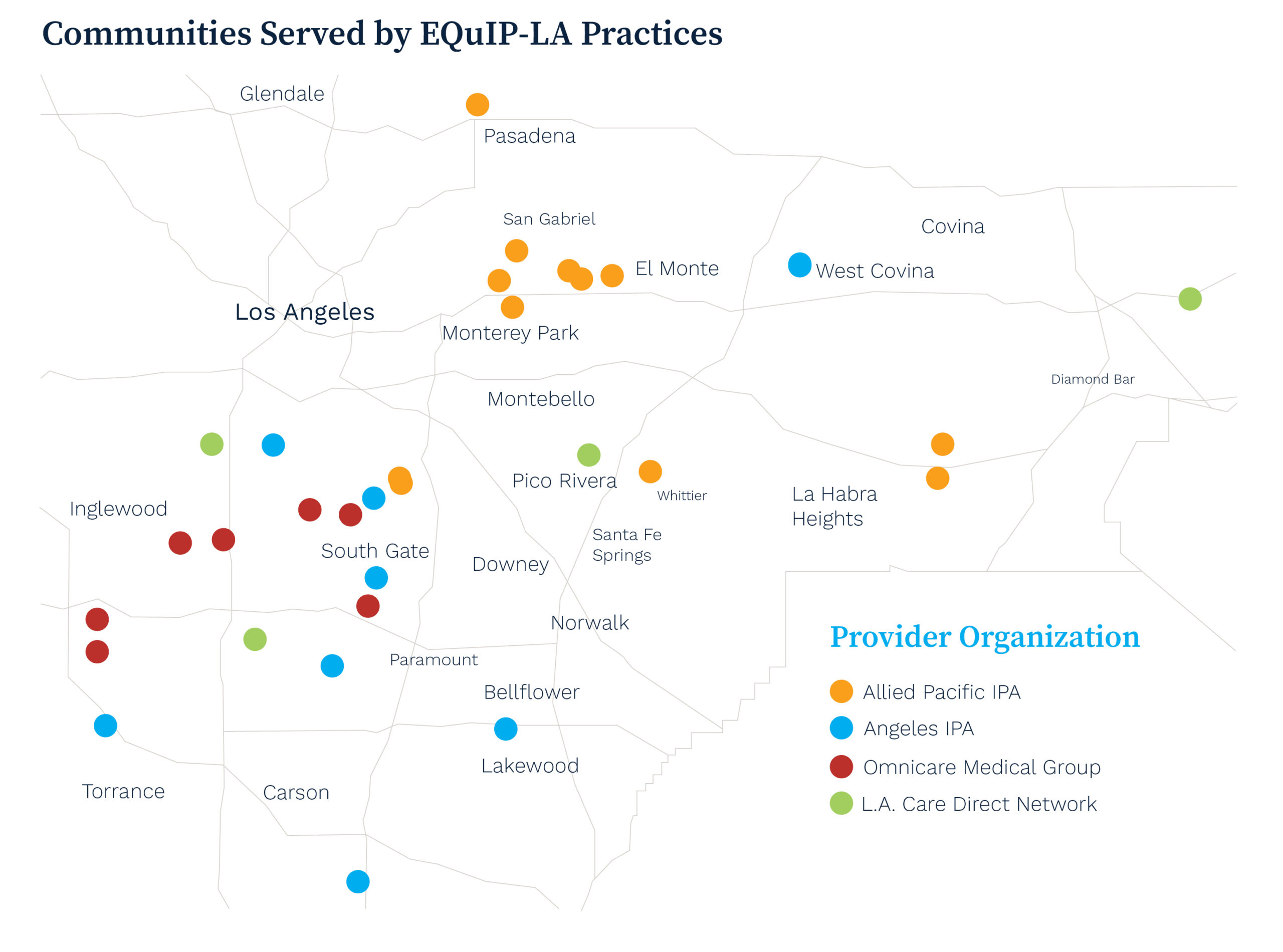
Four organizations committed to advancing health equity are participating in EQuIP-LA, serving more than 41,000 Medi-Cal enrollees, including over 30,000 individuals of color across Los Angeles County:
- Allied Pacific IPA — network of medical professionals serving the San Gabriel Valley
- Angeles IPA — multi-specialty network serving communities across Los Angeles and Orange Counties
- LA. Care Direct Network — directly-contracted network of physicians with L.A. Care Health Plan
- Omnicare Medical Group — multi-specialty network providing quality health care to the citizens of Lynwood, Compton and surrounding communities
Technical Assistance and Impact
EQuIP-LA deploys a community-based coaching model — a scalable approach to build practice coach capacity within health care delivery organizations to help them deliver health equity-focused quality improvement interventions.
Comprehensive technical assistance provided to participants, includes:
- Direct Funding. Supporting infrastructure investments and projects to reduce health disparities for participating IPAs and their enrolled practices.
- Targeted Training. Utilizing evidence-based frameworks to support high-quality primary care, including the Model for Improvement and the 10 Building Blocks of Primary Care.
- Personalized Advising. Offering one-on-one needs assessment and improvement advising to define and implement IPA- and practice-specific quality improvement plans.
- Data Insights. Providing tools to support visualization and interpretation of performance data to identify improvement opportunities.
- Collaborative Learning. Facilitating regular opportunities to engage with peers from other organizations to share learnings and ideas.
Practice Stories of Transformation
The EQuIP-LA program collaborated with primary care practices across Los Angeles County to address disparities in chronic disease management and preventative care.
Tweedy Medical Group credits EQuIP-LA with invigorating their efforts to better serve their patients and greatly expanding their goals.
Reddy Care Medical relied on EQuIP-LA to greatly enhance care coordination and patient follow-up.
Elevating Patients’ Lived Experiences
EQuIP-LA has prioritized patient involvement from its inception, utilizing insights from a virtual patient listening session to inform its strategies. The session, facilitated by CQC and PFCCpartners, allowed Medi-Cal enrollees to share their experiences, directly shaping the program’s focus on timely access and culturally competent care. This approach ensures that interventions are tailored to meet the true needs of the communities served.
The collaborative’s ongoing implementation is supported by a steering committee made up of program partners, participants and a patient representative.
Partners
EQuIP-LA’s technical assistance is led by CQC. Collaborative partners include the California Health Care Foundation, Community Partners, PFCCpartners, HealthBegins, Health Net and L.A. Care Health Plan.
Support
EQuIP-LA is made possible thanks to the generous support of the California Health Care Foundation.
Improvement & Learning Collaboratives
November 7th, 2022
CQC’s improvement and learning collaboratives are multi-year programs offering technical assistance. Program participants receive personalized coaching from experts and engage in educational opportunities including virtual peer sharing, site visits and data analytics. These programs aim to foster a sustainable health care system accessible to all.
CalHIVE Behavioral Health Integration
October 24th, 2022
(more…)
Advanced Primary Care Resources
September 9th, 2022
Employers know that primary care is essential to a healthy workforce and employees’ access to a high-value health care system. Studies show that robust systems of primary care can lower overall health care utilization, disease and death rates and increase the use of preventive services. Strong primary care also may reduce the negative effects of income inequality and is associated with more effective and equitable health services.
For this reason, the Purchaser Business Group on Health (PBGH) has worked for the better part of the last decade to revitalize primary care. Through successive initiatives and in collaboration with a diverse group of committed stakeholders, PBGH has spearheaded efforts to create a blueprint for optimized primary care. The objectives are to fully utilize primary care’s potential to improve health outcomes, integrate behavioral health and reduce costs to the health care system.
Common Measure Set: A set of clearly defined health plan requirements and accountability expectations focused on advanced primary care.
Memorandum of Understanding for Payers: An agreement whereby organizations commit to increase investment in and access to advanced primary care.
Common Purchasing Agreements for Health Plans and Direct Contracting: Purchaser-endorsed standards to help achieve high-value equitable care.
Health Value Index: Specific performance indicators that create actionable insight into a purchaser’s health plan spending.
Advanced Primary Care Request for Information (RFI): PBGH has issued a collective RFI on behalf of our members to identify provider practices that meet established standards of advanced primary care and that are willing to partner. PBGH members will use these results in network design and/or in direct contracting arrangements.
California Advanced Primary Care Initiative
July 25th, 2022
The California Advanced Primary Care Initiative, a joint effort by CQC and the Integrated Healthcare Association (IHA), is a continuation of that effort to strengthen the primary care delivery system throughout the state by building and scaling a primary care model that emphasizes comprehensive, team-based and person-focused care, the integration of behavioral and physical health services and high-quality outcomes.
Multi-Payer Alignment
CQC and the IHA convened a coalition of large commercial health care payers to work together to enable primary care practices to transform to a high-performing, value-based care model that reduces costs and improves quality and equity. The payers currently participating are Aetna, Aledade, Blue Shield of California and Health Net.
These payers have signed a memorandum of understanding (MOU) committing to this coordinated effort through 2025. The MOU has four areas of focus:
1. Transparency: Report primary care investment, adoption of value-based payment models that support the delivery of advanced primary care and performance on the Advanced Primary Care measure set jointly developed by CQC and IHA.
2. Payment: Adopt an agreed upon value-based payment model for primary care providers that offers flexibility, supports team-based care delivery and incentivizes the right care at the right time.
3. Investment: Collaboratively set increased primary care investment quantitative goals without increasing the total cost of care.
4. Practice Transformation: Provide technical assistance to primary care practices working to implement clinical and business models for success in value-based payment models, integration of behavioral health and reduction of disparities.
Additional payer organizations are encouraged to sign onto the MOU and join this effort. Contact Lindsay Petersen to learn more.