Whole-Person, Team-Based Care: Transforming Delivery with BHI Advisory Group Member Dr. Neftali Serrano
August 30th, 2024
Visionaries in Action Series
Members of the California Quality Collaborative (CQC)’s Steering Committee and other committees comprise a diverse group of stakeholders from the health care industry — representing providers, health systems, payers, purchasers, government and advocacy organizations — whose leadership provides strategic direction and guidance for CQC’s quality improvement work to transform the delivery system. These stories offer a glimpse into some of the innovative work of these visionaries.
Dr. Neftali Serrano, Chief Executive Officer of the Collaborative Family Healthcare Association (CFHA), is a leading national advocate for team-based care, particularly in integrating medical and behavioral health providers into a cohesive care team. With over two decades of experience in clinical practice and program development, Dr. Serrano is dedicated to creating a more cohesive and patient-centered health care delivery system. As a member of the California Quality Collaborative (CQC)’s Behavioral Health Integration (BHI) Advisory Group, Dr. Serrano plays a vital role in shaping strategies to accelerate integration of behavioral health into primary care settings for independent California-based practices through CQC’s Behavioral Health Integration Initiative.
A Personal Commitment to Transformative Care
Dr. Serrano’s dedication to integrating behavioral health into primary care is driven by his personal journey and professional experiences. As a Hispanic immigrant from Queens, New York, who grew up in a working-class family without health insurance, he understands the challenges that vulnerable communities face when navigating a fragmented health care system. His early career as a behavioral health provider in a primary care clinic serving underserved families in Chicago highlighted the transformative potential of integrated, team-based care to provide patients with comprehensive medical and behavioral care in a single setting.
“When I started working in a primary care clinic with underserved populations in Chicago, it became clear to me—the power of operating in teams that facilitated seamless service delivery,” Dr. Serrano said. “Patients could see their physician and psychologist in the same visit, in the same room, and we could communicate together about what was needed.”
These experiences have deeply influenced his work at CFHA — an organization focused on supporting health care professionals in integrating physical and behavioral health — and his involvement in the BHI Advisory Group, where he advocates for health care models that are coordinated, accessible, and designed to meet the needs of all patients, especially those from marginalized communities.
Overcoming Challenges in Behavioral Health Integration: California’s Progress
The journey to fully integrating behavioral health into primary care settings in California has been fraught with challenges. Dr. Serrano points to several persistent barriers, including entrenched systems, insufficient training in team-based care and cultural resistance to change within practices and health systems. However, he remains optimistic about the progress being made. Through initiatives like CQC’s CalHIVE BHI improvement collaborative, CFHA, as a technical assistance partner to CQC, is working to address these challenges head-on, starting at the service delivery level and gradually building the necessary infrastructure and training programs to support integrated care. Dr. Serrano believes that making team-based care the centerpiece of health care delivery is key to achieving meaningful and lasting change for patients and providers.
Leveraging Technology for Better Care
A self-proclaimed tech enthusiast, Dr. Serrano is a strong advocate for leveraging digital tools to enhance team-based care. He sees tremendous potential in emerging technologies like artificial intelligence documentation software, which could automate administrative tasks and allow health care providers to spend more time focusing on patient care. Dr. Serrano also emphasizes the need for better measurement tools in behavioral health to enhance care quality. To support the broader adoption of integrated care models and improve patient outcomes across California, CFHA promotes investment in health technology infrastructure. In partnership with CQC, CFHA is advancing these efforts through the Cal-IN Peer Group, a virtual space in which professionals integrating behavioral health into primary care settings in California meet quarterly to connect, share and collaborate.
Looking to the Future: Long-Term Goals for Behavioral Health Integration
Looking ahead, Dr. Serrano is committed to supporting the long-term goals of CQC’s BHI Initiative, which include workforce training, aligning common solutions to support integration implementation and strengthening relationships with managed care organizations. He is particularly excited about CQC’s efforts to align payment and administrative requirements across various payers, a strategy he believes is essential to sustain team-based care. Dr. Serrano views these efforts as a critical step toward creating a more inclusive and effective healthcare system that truly meets everyone’s needs.
Guidance for Providers Seeking to Integrate Behavioral Health
To effectively navigate the complexities of integrating behavioral health services into primary care, Dr. Serrano offers several key recommendations for provider organizations:
- Start small. Implement pilot programs that can be scaled up as they prove successful.
- Build strong partnerships. Collaborate with stakeholders, including health care providers, payers and community organizations, to create a unified approach.
- Secure dedicated funding. Ensure sustainable integration efforts by obtaining financial support specifically allocated for these initiatives.
- Emphasize persistence and patience. Understand that the journey to integrated care is challenging but ultimately rewarding, requiring long-term commitment and resilience.
To learn more about Dr. Serrano’s work and CFHA’s initiatives, visit cfha.net.
Inside CHOC Children’s Well Spaces: School-Based Mental Health in Youth with CQC Steering Committee Member Dr. Mike Weiss
May 30th, 2024
Visionaries in Action Series
Members of the California Quality Collaborative (CQC)’s Steering Committee and other committees comprise a diverse group of stakeholders from the health care industry — representing providers, health systems, payers, purchasers, government and advocacy organizations — whose leadership provides strategic direction and guidance for CQC’s quality improvement work to transform the delivery system. These stories offer a glimpse into some of the innovative work of these visionaries.
PBGH’s California Quality Collaborative (CQC)’s Steering Committee comprises a diverse group of stakeholders from the health care industry — representing providers, health systems, payers, purchasers, government and advocacy organizations — whose leadership provides strategic direction and guidance for CQC’s quality improvement work to transform the delivery system. Dr. Mike Weiss, Vice President of Population Health at Children’s Hospital of Orange County (CHOC), has been a key member of the steering committee for over a decade, four years of which he served as committee co-chair. At CHOC, Dr. Weiss’ team leads the innovative Well Spaces program, a proactive approach to tackling youth mental health challenges within the school environment. This commitment to addressing the growing issue of behavioral health in young patients is also shared by CQC as exemplified by the upcoming launch of the currently recruiting program Behavioral Health Integration – Children and Youth Collaborative Learning Exchange.
The Genesis of Well Spaces
Recognizing the need to shift from reactive to proactive mental health care for youth and understanding that schools are the primary environment for children and families, Dr. Weiss’s team initiated the Well Spaces program. Developed in partnership with the Orange County Department of Education and the CHOC Mental Health Division, this innovative approach aims to deliver mental health support directly in schools, where children spend most of their time — as opposed to hospitals. Well Spaces is part of a multi-pronged effort at CHOC to address a mental health crisis among youth that has reached epidemic proportions. In 2021 more than 1 in 5 (22%) students in the United States seriously considered attempting suicide and 1 in 10 (10%) attempted suicide, according to the Centers for Disease Control and Prevention.
Design and Implementation of Well Spaces
Well Spaces are thoughtfully designed areas within schools that incorporate biophilic design — an architectural approach that connects occupants of a space more closely to nature — to create a calming and therapeutic environment. These spaces are equipped to facilitate stress-reducing activities, such as yoga and mindfulness, offering students proactive mental health interaction. The initiative began with a focus on middle and high schools and has since expanded to 40 locations with plans for more, demonstrating its scalability and effectiveness.
that connects occupants of a space more closely to nature — to create a calming and therapeutic environment. These spaces are equipped to facilitate stress-reducing activities, such as yoga and mindfulness, offering students proactive mental health interaction. The initiative began with a focus on middle and high schools and has since expanded to 40 locations with plans for more, demonstrating its scalability and effectiveness.
Operational Highlights
- Staffing: Each Well Space is staffed by trained school personnel, such as social workers or counselors, ensuring that interventions are appropriately managed. CHOC nurses are available for care coordination as well.
- Student Engagement: Students actively participate in naming and decorating the spaces, fostering a sense of ownership and involvement.
- Integration: The program includes care coordination efforts to help students seamlessly reintegrate into school life after mental health visits to the emergency department or mental health unit.
Strategic Partnerships and Expansion
The success of Well Spaces is bolstered by robust partnerships with stakeholders within the educational system, including formal agreements that facilitate the ongoing involvement and feedback of students — a critical component for the program’s adaptability and growth.
Impact and Evaluations
Dr. Weiss and his team measure the impact of Well Spaces by tracking key indicators such as absenteeism, suspensions and overall school engagement. Initially targeting Title 1 schools, the program has yielded valuable insights into effective strategies for enhancing student mental health, leading to its broader implementation.
Guidance for Providers
Dr. Weiss offers valuable advice for other providers looking to implement similar initiatives:
- Initiate the program at a single school to develop and refine the approach, starting small and scaling up as needed.
- Involve educators, students and parents early to build support and gain momentum, a crucial element for community engagement.
- Obtain dedicated funding sources critical for the program’s long-term success to secure funding and ensure sustainability.
- Understand the local political landscape to align strategies with community expectations and needs, effectively navigating political sensitivity.
Dr. Weiss’s leadership in developing Well Spaces exemplifies the type of innovative thinking that CQC champions as a quality improvement program dedicated to creating lasting, positives change within the health care delivery system. This program not only addresses immediate community needs but also establishes a sustainable model for integrating health care into educational settings.
To learn more about Well Spaces and Dr. Weiss’s work, visit choc.org.
How Primary Care Providers Can Improve Depression Screening
May 4th, 2021
Depression screening is an essential tool for primary care providers to better understand and meet their patients’ needs, especially as behavioral health conditions have dramatically increased in the past year. Patient-centric approaches and thoughtful implementation of depression screening can lead to earlier intervention, improved overall health outcomes and reduced utilization of health care services.
In March 2021, PBGH’s California Quality Collaborative (CQC) hosted a webinar on the importance of depression screening for patients, providers and payers and shared practical advice for patient-centered depression screening. Experts from PBGH, Montefiore Medical Center and UCLA identified four key takeaways during the discussion:
1. Primary care providers should start screening patients for depression now. There is increasing demand being placed on primary care clinicians to screen patients for depression. Health plans, employers and other purchasers of health care recognize that depression affects millions of patients, and they are investing in behavioral health as a strategy to improve health outcomes. In California, there is momentum from organizations like the Integrated Healthcare Association, which runs statewide performance improvement programs, and Covered California, to include depression screening as a required health care quality measure. Providers will be financially accountable for completing depression screening in the next several years as part of existing pay-for-performance programs.
2. Care teams need training to be comfortable screening patients for depression. Care teams require resources and information about depression screening and how to follow up appropriately with patients in need of behavioral health services. Specialized trainings with role-playing opportunities are effective, as are resources, such as a list of frequently asked questions developed by the Advancing Integrated Mental Health Solution (AIMS) Center from University of Washington.
3. Screening workflows can be integrated into virtual visits, with intentional planning. During the public health emergency, UCLA Health increased the use of virtual primary care visits. The system’s clinical and operations teams created a depression screening workflow that leveraged “virtual rooming” steps, during which clinical support staff register and prepare patients for telehealth visits just as they would for in-person clinical appointments. To address safety concerns associated with suicidal ideation documented in patient depression questionnaires, they tested and implemented several solutions by which the provider would monitor a patient’s response, or the electronic health record would issue an automatic alert.
4. Technology can expand the reach of primary care to provide whole-person care. Montefiore Medical Center launched a smartphone app that includes screening, educational resources, appointment and medication reminders and near real-time chat, among other features. Providers using the Montefiore app with their patients found that it improved behavioral health care engagement with a diverse set of patient populations. In an analysis of the smartphone app pilot data, 72% of patients used it to access educational articles and videos, 69% used it to interact with their care teams via secure chat or text and 67% used the app to complete a depression or other behavioral screening scale.
For additional insights about how primary care providers can improve depression screening for their patients, watch the March 31 CQC webinar or access the presentation.
The Current State of Mental Health Screening and Access in California: Results from 35,000 Patients
October 26th, 2020
Mental health concerns are increasingly common, yet many patients in California are not screened for symptoms and are unable to access treatment. Understanding patients’ access to care is challenging; data are scarce and usually only available at a statewide level, even though there are likely wide regional differences due to workforce shortages.
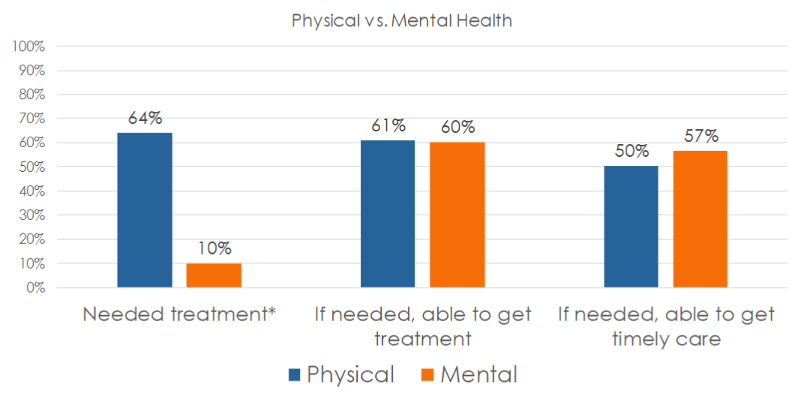
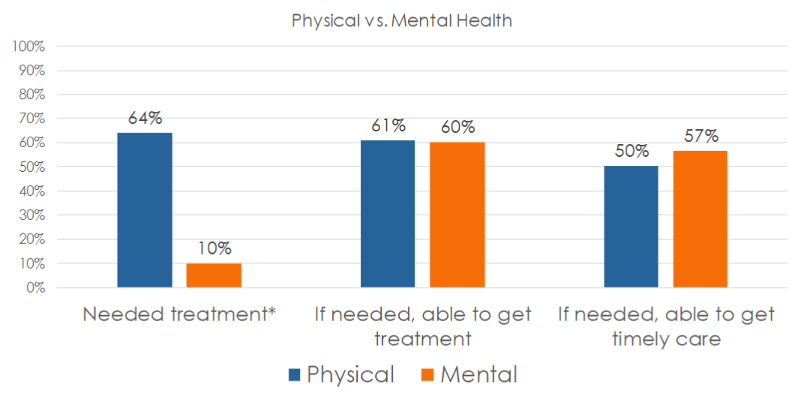
In its Accelerating Integrated Care webinar series , the Pacific Business Group on Health’s (PBGH) California Quality Collaborative presented results from the most recent PBGH Patient Assessment Survey (PAS). The research measured the experience of 35,000 Californians regarding mental health screening and access to necessary treatment. Also measured was the degree to which patients were successful getting timely access to physical versus mental health care.
Screening Rates and Access to Mental Health Treatment are Low
Participants of the survey visited either a primary care or specialty medical provider between July and October of 2019 and were asked to rate their experiences with their medical care during the six months prior to receiving the survey. Survey participants were asked a series of questions, including:
- Were you asked about mental health symptoms during your medical visit during the past six months?
- Was treatment recommended?
- Did you need treatment?
- Were you able to get care?
- Were you able to get care when you needed it?
Many patients (67%) said that no one from their provider’s office – whether a primary care or specialist visit — had asked them about their mental health, despite 16% reporting feeling they needed care and 30% having accessed care on their own. One-third (33%) said a provider asked them about their mental health.
Half of all patients who were screened were recommended for mental health treatment. Two-thirds agreed they needed the care that was recommended.

Whether in need of mental or physical health care, 60% of those surveyed said they were always able to get access to needed services. Surprisingly, a higher percentage of survey participants in need of mental health services (57%) said they were able to get care when they needed it, compared to just 50% seeking physical health services.
Using Patient Reported Data to Improve Access to Mental Health Care
All provider organizations can utilize this data to improve upon the rate at which patients are screened for mental health symptoms and to ensure they gain access to needed care. Using either baseline data or the Patient Assessment Survey data presented here as a proxy, comparisons against state benchmarks to set goals for screening and access can be made. To begin improvement work, select evidence-based change tactics to create an action plan.
It is important to ask patients about their experiences accessing care at your organization. Encounter and claims data can be useful in instances when patients who have been seen for a medical appointment have also filled out a screening tool, though this data do not capture whether the patient was satisfied with their experience and felt they received care when they needed it. Follow the steps below to capture feedback from patients to identify populations that might need extra support.
If your organization does not already collect such data:
- Measure: Develop a survey to collect patient data.
- Interpret: Use the data presented in this article as a proxy benchmark until you collect your own data – assume your screening and access rates are similar (33% screened, 60% able to access care).
If your organization already collects patient experience data for mental health care:
- Measure: Identify a contact at your organization who can provide data on mental health screening and access.
- Interpret: Compare your internal data to the statewide data presented in this webinar (33% screened, 60% able to access care) – how does your organization compare? Which populations might need extra support?
For more details on upcoming CQC webinars focusing on how to improve mental health screenings and access to mental health treatment in primary care settings, sign up for the CQC Newsletter or visit the Webinars webpage . Later this year, PBGH will publish an Issue Brief with further results from this study. For more information, find the full recording of this webinar here and the slide deck here.
 that connects occupants of a space more closely to nature — to create a calming and therapeutic environment. These spaces are equipped to facilitate stress-reducing activities, such as yoga and mindfulness, offering students proactive mental health interaction. The initiative began with a focus on middle and high schools and has since expanded to 40 locations with plans for more, demonstrating its scalability and effectiveness.
that connects occupants of a space more closely to nature — to create a calming and therapeutic environment. These spaces are equipped to facilitate stress-reducing activities, such as yoga and mindfulness, offering students proactive mental health interaction. The initiative began with a focus on middle and high schools and has since expanded to 40 locations with plans for more, demonstrating its scalability and effectiveness.